
- Bipolar Disorder

New Study Gives an Important Update on Bipolar Disorder
A recent paper summarizes valuable information about bipolar disorder and its treatment..
Posted December 11, 2023 | Reviewed by Devon Frye
- What Is Bipolar Disorder?
- Take our Bipolar Disorder Test
- Find counselling to treat bipolar disorder
- Worldwide, over 2.5% of the population will have either bipolar I or bipolar II during their lifetimes.
- These illnesses are associated with a greater than 10-year decrease in life span. Death by suicide is common.
- Medications are helpful, but they can have long-term side effects.
- Lithium treatment is associated with decreases in the suicide rate and all-cause mortality.
Bipolar disorders are characterized by episodes of mania, hypomania , and depression . DSM-5-TR (the Diagnostic and Statistical Manual of Mental Disorders ) defines a manic episode as a “distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary).” Manic symptoms include inflated self-esteem , decreased need for sleep, racing thoughts and/or speech, distractibility, agitation, and impaired judgment.
Manic episodes cause social and occupational impairment and can have psychotic features. Hypomanic episodes have similar symptoms but are less severe and by definition do not require hospitalization or have psychotic features.
Individuals with bipolar I disorder have a history of manic episodes that interfere with function or necessitate hospitalization. In addition to manic episodes, depressive episodes are common. Those with bipolar II disorder have milder hypomanic symptoms/episodes in addition to major depressive episodes.
Andrew Nierenberg and colleagues recently published a review article in the Journal of the American Medical Association (JAMA) about the diagnosis and treatment of bipolar disorder . Some of this information may not be well known, and we thought it would be useful to summarize a few important points.
Bipolar disorder is common. Approximately 1 percent of the world’s population will have bipolar I disorder during their lifetimes, and over 1.5 percent will have bipolar II disorder. In the U.S., the combined percentage may be higher—up to 4 percent or more.
The consequences of these disorders are substantial. As we mentioned in an earlier post , bipolar disorder is associated with premature mortality. Life expectancy is decreased by 12-14 years. The authors note that about 34 percent of individuals with bipolar disorder attempt suicide and over 15 percent take their own lives.
Individuals with bipolar disorder experience more time suffering from depressive episodes than manic episodes. Depressive episodes account for 75 percent of symptomatic time.
Bipolar disorder is associated with comorbid psychiatric disorders. The two most common are anxiety disorders, occurring in over 70 percent of individuals with bipolar disorder, and substance use disorders, occurring in about 56 percent.
Pharmacotherapy is the mainstay of treatment. Various psychotherapies and lifestyle changes are also helpful.
Lithium, mood-stabilizing anticonvulsants, and antipsychotics are the three classes of drugs utilized in treating bipolar disorder. These drugs are often used in various combinations. Pharmacologic treatment varies depending on the stage of illness, i.e., acute treatment may require different pharmacological approaches than treatment to maintain remission of symptoms.
Electroconvulsive therapy (ECT) can be effective for treating symptoms of bipolar depression that are resistant to medications. Over 75 percent of people respond to ECT, and in over 50 percent, symptoms remit. However, follow-up treatments are needed to decrease the risk of relapse .
The review article also discusses information related to various drugs. Here are a few details about lithium and antipsychotics that may not be well-known:
- Lithium can be helpful both in the acute and maintenance phases of treatment. In addition to side effects such as hypothyroidism (treatable with thyroid medication), clinically significant decreases in kidney function can occur in those taking lithium long-term. Kidney function should be routinely monitored.
- Lithium is associated with a substantial (over 70 percent) decrease in suicide rate and a major decrease in all-cause mortality, decreasing it by more than half.
- Antipsychotics are helpful in both the acute and maintenance phases of the illness. There can be cardiovascular, metabolic, and movement disorder side effects that vary depending on the specific drug.
- Antipsychotics are associated with a dose-dependent increase in 5-year mortality ranging from a 13 percent increase with lower doses to a 69 percent increase with moderate doses to an over 2-fold increase with high doses.
To summarize, bipolar disorder is a common illness with serious functional, social, medical, and psychiatric consequences. Individuals can be helped by various pharmacologic interventions, lifestyle changes, and psychotherapies. There are different considerations in selecting specific medications.
Much more research is needed to better understand this disorder and to develop preventative and therapeutic interventions.

This column was written by Eugene Rubin, M.D., Ph.D., and Charles Zorumski, M.D.
Nierenberg, A.A., Agustini, B., Kohler-Forsberg, O., Cusin, C., Katz, D., Sylvia, L.G., Peters, A., & Berk, M. (2023 Oct 10). Diagnosis and treatment of bipolar disorder: a review. JAMA. 330(14):1370-1380. doi: 10.1001/jama.2023.18588.

Eugene Ru bin , M.D., Ph.D. , is Professor Emeritus in the Department of Psychiatry at Washington University School of Medicine in St. Louis.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

- BD² Integrated Network
Discovery Research
Brain omics platform, genetics platform.
- RFA Opportunities
- Current Grantees
- About Bipolar Disorder
- Scientific Steering Committees
- Philanthropic Investors
- BD² Updates
Funding Availability
BD² seeks multidisciplinary teams to collaborate and explore the fundamental mechanisms, heterogeneity, progression, and underlying biology of bipolar disorder.

Driving Discovery
BD 2 is the first organization focused on funding and advancing research and care for bipolar disorder on a global scale.

Shortening Diagnosis to Treatment Time
We engage people with lived experience and collect data in real-world clinical settings to advance the scientific understanding of bipolar disorder and improve care.

Accelerating Bipolar Disorder Science
We are forging research pathways to lift the ceiling on scientific understanding and to create new interventions so that everyone with bipolar disorder can thrive.

Data Discovery
Connecting Experience

Revolutionized Systems
Focusing science on the greatest impact for people.
Current research, treatment, and care for bipolar disorder lacks scientific precision of the disorder and its diversity. We aim to change that.
Current State
- It takes 7 years on average to diagnose bipolar disorder.
- It takes 17 years on average to translate a scientific discovery to meaningful interventions for people with bipolar disorder.
- Fewer than 50% of individuals find effective treatments.
What BD² is Doing
- Researching previously unknown scientific foundations of bipolar disorder, including biological indicators and genetic mechanisms.
- Building the largest collaborative scientific network for bipolar disorder focused on applying learnings to evidence-based, personalized treatment.
- Collecting and sequencing the largest and most diverse set of brain samples to expand the understanding of the disorder.
Future State
- A bipolar diagnosis is identifiable at the onset of proven genetic and biological markers.
- Evidence-based treatments are discovered, and improved outcomes are possible for people with bipolar disorder within a short time of diagnosis.
- All people with bipolar disorder manage the disorder effectively and thrive in their lives.
Four Interconnected Programs, Zero Silos
Our mission is to accelerate scientific understanding of bipolar disorder and advance clinical care through cross-disciplinary collaboration, data sharing, and real-time learning.
Integrated Network
Bridge Insight With Precision Psychiatry
Discover the Biological Pathways
Understand the Differences in the Brain
Uncover the Genetic Contributions
Our comprehensive, hypothesis-driven approach breaks down barriers between innovation, scientific findings, and clinical care.

News & Updates

September 26, 2024
Washington, D.C. – BD²: Breakthrough Discoveries for thriving with Bipolar Disorder today…

September 12, 2024
When BD²’s Integrated Network set out to build its groundbreaking approach to shorten the time…
August 22, 2024
A Learning Health Network is a relatively new, innovative concept that brings healthcare delivery…

August 7, 2024
The BD² Integrated Network is a groundbreaking approach designed to shorten the time it takes for…

July 18, 2024
Washington, D.C. – July 18, 2024 – BD²: Breakthrough Discoveries for thriving with Bipolar…
March 29, 2024
BD² recognizes World Bipolar Day as a reminder of our shared vision: that all people with bipolar…
Cultivating the power of collaboration.
BD 2 is invested in the talent of our people and partners, fostering team development and connection across the network.
" The wonder of science is that while we can’t know where new discovery will come from, we can stack the deck in our favor and aim it towards the greatest impact for people."

Engage & Connect With Us Today
Join us in achieving the vision of a world where all people with bipolar disorder thrive.
Receive Updates
Apply for funding, thrive updates.
Sign up to receive our emails with the latest information on funding availability, research findings, and more.
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Listening Meetings
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Terms, Privacy & Notices
- Dept. Diversity Vice Chairs & Champions
- DEI Educational Offerings
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Individual Resources
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- House Naming Process
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Faculty Facing Caregiving Need
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Faculty Attestation
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Faculty & Staff
- Issues List
- Print Magazine PDFs
- Archive of Issues List
- Archive of Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- YSM & the Community
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Investigators Launch Study Aimed at Accelerating Understanding of Bipolar Disorder
A multidisciplinary team of researchers based at Yale will launch a series of studies aimed at accelerating understanding of bipolar disorder and generating new and more effective treatments.
Together with Harvard University, Stanford University , and the New York Genome Center, Yale will be one of four sites funded by $18 million in research grants from BD²: Breakthrough Discoveries for Thriving with Bipolar Disorder , a research funding initiative that brings together researchers, clinicians, philanthropists, and people with lived experience to study and treat bipolar disorder.
The unprecedented opportunities for researchers to perform this work in the context of the highly collaborative larger BD² network, we think, have potential to be transformative. Hilary Blumberg, MD
Each site will receive grants of up to $4.5 million from the BD² Discovery Research program over three years to examine the fundamental mechanisms of bipolar disorder.
Yale’s research team will be led by Hilary Blumberg, MD , John and Hope Furth Professor of Psychiatric Neuroscience and Professor of Psychiatry, and in the Child Study Center and of Radiology and Biomedical Imaging. Blumberg directs Yale School of Medicine’s Mood Disorders Research Program; her research is devoted to understanding the brain circuitry differences that underlie mood disorders across the lifespan, with a focus on bipolar disorder and suicide prevention.
“The Discovery Research program is the cornerstone of BD²’s work to improve understanding so that we can more effectively diagnose and improve treatment for the tens of millions of people living with bipolar disorder,” said Cara Altimus, PhD, managing director for BD² and senior director at the Milken Institute. “These teams of scientists will work within their own institutions and collaborate across teams to explore hypotheses on the biological causes of bipolar disorder.”
Blumberg will lead her team to investigate the roles of mitochondria, the energy powerhouses of cells, in the brain in bipolar disorder and how they can lead to the low-energy symptoms of depression and high-energy symptoms of mania.
In a unique multidisciplinary effort, they will study mitochondria from their basic genetic and molecular mechanisms to how they change brain-cell metabolism and functioning, to how they affect brain-circuitry functioning and symptoms. These studies will expand knowledge about bipolar-disorder biology. Importantly, they will translate their findings into pharmacological therapeutics and behavioral interventions.
This work will be divided into four projects, or “aims;” each will have a unique focus and will contribute to Yale’s overall integrated multidisciplinary research approach.
Blumberg is both the project’s principal investigator and lead on Aim 1. Researchers in her group will perform extensive characterization of people with bipolar disorder, including details of clinical, behavioral, and psychosocial risk factors, and will use new multimodal brain-scanning methods to study brain-system function and metabolism.
In-Hyun Park, PhD , associate professor of genetics, will lead Aim 2 in which, from the blood samples of participants in Aim 1, he will generate and study stem cells and “brain organoids.” This will allow for study of each individual’s brain cell physiology and its response to specific treatments.
Aim 3’s intensive mitochondrial study will be led by Elizabeth Jonas, MD , Harvey and Kate Cushing Professor of Medicine, who was a discoverer of the mitochondrial mechanism that will be the focus of the work.
Hongying Shen, PhD , assistant professor of cellular and molecular physiology, will use state-of-the-art CRISPR methods to study mitochondrial genetic mechanisms in leading Aim 4. Other Yale scientists collaborating with in this study include K risten Brennand, PhD ; T odd Constable, PhD ; Irina Esterlis, PhD ; Joy Hirsch, PhD ; and Graeme Mason, PhD , who will be joined by University College of London Professor in Biomedical Engineering Ilias Tachtsidis , PhD.
“This support from BD² will provide us unique opportunities to study the same individuals with bipolar disorder with new ways to scan their brains to examine brain-circuitry function and metabolism and, in brain cells derived with recent stem cell technologies from their blood samples, study individual genetic and molecular mechanisms involved and how they respond to specific medications,” Blumberg said. “The unprecedented opportunities for researchers to perform this work in the context of the highly collaborative larger BD² network, we think, have potential to be transformative in elucidating causes of BD and in generating more effective diagnostic and treatment methods.”
- Basic Science Research
Featured in this article
- Hilary Blumberg, MD John and Hope Furth Professor of Psychiatric Neuroscience and Professor of Psychiatry, and in the Child Study Center and of Radiology and Biomedical Imaging; Director, Mood Disorders Research Program
- In-Hyun Park, PhD Associate Professor of Genetics; Yale Stem Cell Center
- Elizabeth Jonas, MD Harvey and Kate Cushing Professor of Medicine (Endocrinology) and Professor of Neuroscience
- Hongying Shen, PhD Assistant Professor of Cellular and Molecular Physiology
- Kristen Brennand, PhD Elizabeth Mears and House Jameson Professor of Psychiatry; Co-director, Science Fellows Program
- Todd Constable, PhD Elizabeth Mears and House Jameson Professor of Radiology and Biomedical Imaging and Professor of Neurosurgery; Co-Director MRI Research Center, Magnetic Resonance Imaging
- Irina Esterlis, PhD Professor of Psychiatry; Director, Molecular Imaging Program, NCPTSD, VA; Director, Mood, Anxiety, and Cognitive Sciences Division
- Joy Hirsch, PhD Elizabeth Mears and House Jameson Professor of Psychiatry and Professor of Comparative Medicine and of Neuroscience
- Graeme Mason, PhD Professor of Radiology and Biomedical Imaging and of Psychiatry; Director Metabolic Modeling and Director Psychiatric MRS, Magnetic Resonance Research Center; Director, Neuroimaging Sciences Training Program, Radiology & Biomedical Imaging and Psychiatry; Chair, Magnetic Resonance Research Center Protocol Review Committee, Radiology & Biomedical Imaging
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 17 May 2021
Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology
- Niamh Mullins ORCID: orcid.org/0000-0001-8021-839X 1 , 2 na1 ,
- Andreas J. Forstner 3 , 4 , 5 na1 ,
- Kevin S. O’Connell 6 , 7 ,
- Brandon Coombes 8 ,
- Jonathan R. I. Coleman 9 , 10 ,
- Zhen Qiao 11 ,
- Thomas D. Als 12 , 13 , 14 ,
- Tim B. Bigdeli 15 , 16 ,
- Sigrid Børte 17 , 18 , 19 ,
- Julien Bryois 20 ,
- Alexander W. Charney 2 ,
- Ole Kristian Drange 21 , 22 ,
- Michael J. Gandal 23 ,
- Saskia P. Hagenaars 9 , 10 ,
- Masashi Ikeda 24 ,
- Nolan Kamitaki 25 , 26 ,
- Minsoo Kim 23 ,
- Kristi Krebs 27 ,
- Georgia Panagiotaropoulou 28 ,
- Brian M. Schilder 1 , 29 , 30 , 31 ,
- Laura G. Sloofman 1 ,
- Stacy Steinberg 32 ,
- Vassily Trubetskoy 28 ,
- Bendik S. Winsvold 19 , 33 ,
- Hong-Hee Won 34 ,
- Liliya Abramova 35 ,
- Kristina Adorjan 36 , 37 ,
- Esben Agerbo 14 , 38 , 39 ,
- Mariam Al Eissa 40 ,
- Diego Albani 41 ,
- Ney Alliey-Rodriguez 42 , 43 ,
- Adebayo Anjorin 44 ,
- Verneri Antilla 45 ,
- Anastasia Antoniou 46 ,
- Swapnil Awasthi 28 ,
- Ji Hyun Baek 47 ,
- Marie Bækvad-Hansen 14 , 48 ,
- Nicholas Bass 40 ,
- Michael Bauer 49 ,
- Eva C. Beins 3 ,
- Sarah E. Bergen 20 ,
- Armin Birner 50 ,
- Carsten Bøcker Pedersen 14 , 38 , 39 ,
- Erlend Bøen 51 ,
- Marco P. Boks 52 ,
- Rosa Bosch 53 , 54 , 55 , 56 ,
- Murielle Brum 57 ,
- Ben M. Brumpton 19 ,
- Nathalie Brunkhorst-Kanaan 57 ,
- Monika Budde 36 ,
- Jonas Bybjerg-Grauholm 14 , 48 ,
- William Byerley 58 ,
- Murray Cairns 59 ,
- Miquel Casas 53 , 54 , 55 , 56 ,
- Pablo Cervantes 60 ,
- Toni-Kim Clarke 61 ,
- Cristiana Cruceanu 60 , 62 ,
- Alfredo Cuellar-Barboza 63 , 64 ,
- Julie Cunningham 65 ,
- David Curtis 66 , 67 ,
- Piotr M. Czerski 68 ,
- Anders M. Dale 69 ,
- Nina Dalkner 50 ,
- Friederike S. David 3 ,
- Franziska Degenhardt 3 , 70 ,
- Srdjan Djurovic 71 , 72 ,
- Amanda L. Dobbyn 1 , 2 ,
- Athanassios Douzenis 46 ,
- Torbjørn Elvsåshagen 18 , 73 , 74 ,
- Valentina Escott-Price 75 ,
- I. Nicol Ferrier 76 ,
- Alessia Fiorentino 40 ,
- Tatiana M. Foroud 77 ,
- Liz Forty 75 ,
- Josef Frank 78 ,
- Oleksandr Frei 6 , 18 ,
- Nelson B. Freimer 23 , 79 ,
- Louise Frisén 80 ,
- Katrin Gade 36 , 81 ,
- Julie Garnham 82 ,
- Joel Gelernter 83 , 84 , 85 ,
- Marianne Giørtz Pedersen 14 , 38 , 39 ,
- Ian R. Gizer 86 ,
- Scott D. Gordon 87 ,
- Katherine Gordon-Smith 88 ,
- Tiffany A. Greenwood 89 ,
- Jakob Grove 12 , 13 , 14 , 90 ,
- José Guzman-Parra 91 ,
- Kyooseob Ha 92 ,
- Magnus Haraldsson 93 ,
- Martin Hautzinger 94 ,
- Urs Heilbronner 36 ,
- Dennis Hellgren 20 ,
- Stefan Herms 3 , 95 , 96 ,
- Per Hoffmann 3 , 95 , 96 ,
- Peter A. Holmans 75 ,
- Laura Huckins 1 , 2 ,
- Stéphane Jamain 97 , 98 ,
- Jessica S. Johnson 1 , 2 ,
- Janos L. Kalman 36 , 37 , 99 ,
- Yoichiro Kamatani 100 , 101 ,
- James L. Kennedy 102 , 103 , 104 , 105 ,
- Sarah Kittel-Schneider 57 , 106 ,
- James A. Knowles 107 , 108 ,
- Manolis Kogevinas 109 ,
- Maria Koromina 110 ,
- Thorsten M. Kranz 57 ,
- Henry R. Kranzler 111 , 112 ,
- Michiaki Kubo 113 ,
- Ralph Kupka 114 , 115 , 116 ,
- Steven A. Kushner 117 ,
- Catharina Lavebratt 118 , 119 ,
- Jacob Lawrence 120 ,
- Markus Leber 121 ,
- Heon-Jeong Lee 122 ,
- Phil H. Lee 123 ,
- Shawn E. Levy 124 ,
- Catrin Lewis 75 ,
- Calwing Liao 125 , 126 ,
- Susanne Lucae 62 ,
- Martin Lundberg 118 , 119 ,
- Donald J. MacIntyre 127 ,
- Sigurdur H. Magnusson 32 ,
- Wolfgang Maier 128 ,
- Adam Maihofer 89 ,
- Dolores Malaspina 1 , 2 ,
- Eirini Maratou 129 ,
- Lina Martinsson 80 ,
- Manuel Mattheisen 12 , 13 , 14 , 106 , 130 ,
- Steven A. McCarroll 25 , 26 ,
- Nathaniel W. McGregor 131 ,
- Peter McGuffin 9 ,
- James D. McKay 132 ,
- Helena Medeiros 108 ,
- Sarah E. Medland 87 ,
- Vincent Millischer 118 , 119 ,
- Grant W. Montgomery 11 ,
- Jennifer L. Moran 25 , 133 ,
- Derek W. Morris 134 ,
- Thomas W. Mühleisen 4 , 95 ,
- Niamh O’Brien 40 ,
- Claire O’Donovan 82 ,
- Loes M. Olde Loohuis 23 , 79 ,
- Lilijana Oruc 135 ,
- Sergi Papiol 36 , 37 ,
- Antonio F. Pardiñas 75 ,
- Amy Perry 88 ,
- Andrea Pfennig 49 ,
- Evgenia Porichi 46 ,
- James B. Potash 136 ,
- Digby Quested 137 , 138 ,
- Towfique Raj 1 , 29 , 30 , 31 ,
- Mark H. Rapaport 139 ,
- J. Raymond DePaulo 136 ,
- Eline J. Regeer 140 ,
- John P. Rice 141 ,
- Fabio Rivas 91 ,
- Margarita Rivera 142 , 143 ,
- Julian Roth 106 ,
- Panos Roussos 1 , 2 , 29 ,
- Douglas M. Ruderfer 144 ,
- Cristina Sánchez-Mora 53 , 54 , 56 , 145 ,
- Eva C. Schulte 36 , 37 ,
- Fanny Senner 36 , 37 ,
- Sally Sharp 40 ,
- Paul D. Shilling 89 ,
- Engilbert Sigurdsson 93 , 146 ,
- Lea Sirignano 78 ,
- Claire Slaney 82 ,
- Olav B. Smeland 6 , 7 ,
- Daniel J. Smith 147 ,
- Janet L. Sobell 148 ,
- Christine Søholm Hansen 14 , 48 ,
- Maria Soler Artigas 53 , 54 , 56 , 145 ,
- Anne T. Spijker 149 ,
- Dan J. Stein 150 ,
- John S. Strauss 102 ,
- Beata Świątkowska 151 ,
- Chikashi Terao 101 ,
- Thorgeir E. Thorgeirsson 32 ,
- Claudio Toma 152 , 153 , 154 ,
- Paul Tooney 59 ,
- Evangelia-Eirini Tsermpini 110 ,
- Marquis P. Vawter 155 ,
- Helmut Vedder 156 ,
- James T. R. Walters 75 ,
- Stephanie H. Witt 78 ,
- Simon Xi 157 ,
- Wei Xu 158 ,
- Jessica Mei Kay Yang 75 ,
- Allan H. Young 159 , 160 ,
- Hannah Young 1 ,
- Peter P. Zandi 136 ,
- Hang Zhou 83 , 84 ,
- Lea Zillich 78 ,
- HUNT All-In Psychiatry ,
- Rolf Adolfsson 161 ,
- Ingrid Agartz 51 , 130 , 162 ,
- Martin Alda 82 , 163 ,
- Lars Alfredsson 164 ,
- Gulja Babadjanova 165 ,
- Lena Backlund 118 , 119 ,
- Bernhard T. Baune 166 , 167 , 168 ,
- Frank Bellivier 169 , 170 ,
- Susanne Bengesser 50 ,
- Wade H. Berrettini 171 ,
- Douglas H. R. Blackwood 61 ,
- Michael Boehnke 172 ,
- Anders D. Børglum 14 , 173 , 174 ,
- Gerome Breen 9 , 10 ,
- Vaughan J. Carr 175 ,
- Stanley Catts 176 ,
- Aiden Corvin 177 ,
- Nicholas Craddock 75 ,
- Udo Dannlowski 166 ,
- Dimitris Dikeos 178 ,
- Tõnu Esko 26 , 27 , 179 , 180 ,
- Bruno Etain 169 , 170 ,
- Panagiotis Ferentinos 9 , 46 ,
- Mark Frye 64 ,
- Janice M. Fullerton 152 , 153 ,
- Micha Gawlik 106 ,
- Elliot S. Gershon 42 , 181 ,
- Fernando S. Goes 136 ,
- Melissa J. Green 152 , 175 ,
- Maria Grigoroiu-Serbanescu 182 ,
- Joanna Hauser 68 ,
- Frans Henskens 59 ,
- Jan Hillert 80 ,
- Kyung Sue Hong 47 ,
- David M. Hougaard 14 , 48 ,
- Christina M. Hultman 20 ,
- Kristian Hveem 19 , 183 ,
- Nakao Iwata 24 ,
- Assen V. Jablensky 184 ,
- Ian Jones 75 ,
- Lisa A. Jones 88 ,
- René S. Kahn 2 , 52 ,
- John R. Kelsoe 89 ,
- George Kirov 75 ,
- Mikael Landén 20 , 185 ,
- Marion Leboyer 97 , 98 , 186 ,
- Cathryn M. Lewis 9 , 10 , 187 ,
- Qingqin S. Li 188 ,
- Jolanta Lissowska 189 ,
- Christine Lochner 190 ,
- Carmel Loughland 59 ,
- Nicholas G. Martin 87 , 191 ,
- Carol A. Mathews 192 ,
- Fermin Mayoral 91 ,
- Susan L. McElroy 193 ,
- Andrew M. McIntosh 127 , 194 ,
- Francis J. McMahon 195 ,
- Ingrid Melle 6 , 196 ,
- Patricia Michie 59 ,
- Lili Milani 27 ,
- Philip B. Mitchell 175 ,
- Gunnar Morken 21 , 197 ,
- Ole Mors 14 , 198 ,
- Preben Bo Mortensen 12 , 14 , 38 , 39 ,
- Bryan Mowry 176 ,
- Bertram Müller-Myhsok 62 , 199 , 200 ,
- Richard M. Myers 124 ,
- Benjamin M. Neale 25 , 45 , 179 ,
- Caroline M. Nievergelt 89 , 201 ,
- Merete Nordentoft 14 , 202 ,
- Markus M. Nöthen 3 ,
- Michael C. O’Donovan 75 ,
- Ketil J. Oedegaard 203 , 204 ,
- Tomas Olsson 205 ,
- Michael J. Owen 75 ,
- Sara A. Paciga 206 ,
- Chris Pantelis 207 ,
- Carlos Pato 108 ,
- Michele T. Pato 108 ,
- George P. Patrinos 110 , 208 , 209 ,
- Roy H. Perlis 210 , 211 ,
- Danielle Posthuma 212 , 213 ,
- Josep Antoni Ramos-Quiroga 53 , 54 , 55 , 56 ,
- Andreas Reif 57 ,
- Eva Z. Reininghaus 50 ,
- Marta Ribasés 53 , 54 , 56 , 145 ,
- Marcella Rietschel 78 ,
- Stephan Ripke 25 , 28 , 45 ,
- Guy A. Rouleau 126 , 214 ,
- Takeo Saito 24 ,
- Ulrich Schall 59 ,
- Martin Schalling 118 , 119 ,
- Peter R. Schofield 152 , 153 ,
- Thomas G. Schulze 36 , 78 , 81 , 136 , 215 ,
- Laura J. Scott 172 ,
- Rodney J. Scott 59 ,
- Alessandro Serretti 216 ,
- Cynthia Shannon Weickert 152 , 175 , 217 ,
- Jordan W. Smoller 25 , 133 , 218 ,
- Hreinn Stefansson 32 ,
- Kari Stefansson 32 , 219 ,
- Eystein Stordal 220 , 221 ,
- Fabian Streit 78 ,
- Patrick F. Sullivan 20 , 222 , 223 ,
- Gustavo Turecki 224 ,
- Arne E. Vaaler 225 ,
- Eduard Vieta 226 ,
- John B. Vincent 102 ,
- Irwin D. Waldman 227 ,
- Thomas W. Weickert 152 , 175 , 217 ,
- Thomas Werge 14 , 228 , 229 , 230 ,
- Naomi R. Wray 11 , 231 ,
- John-Anker Zwart 18 , 19 , 33 ,
- Joanna M. Biernacka 8 , 64 ,
- John I. Nurnberger 232 ,
- Sven Cichon 3 , 4 , 95 , 96 ,
- Howard J. Edenberg 77 , 233 ,
- Eli A. Stahl 1 , 2 , 179 na2 ,
- Andrew McQuillin 40 na2 ,
- Arianna Di Florio 75 , 223 na2 ,
- Roel A. Ophoff 23 , 79 , 117 , 234 na2 &
- Ole A. Andreassen ORCID: orcid.org/0000-0002-4461-3568 6 , 7 na2
Nature Genetics volume 53 , pages 817–829 ( 2021 ) Cite this article
42k Accesses
587 Citations
322 Altmetric
Metrics details
- Bipolar disorder
- Genome-wide association studies
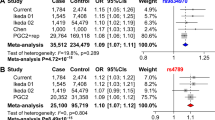
Bipolar disorder is a heritable mental illness with complex etiology. We performed a genome-wide association study of 41,917 bipolar disorder cases and 371,549 controls of European ancestry, which identified 64 associated genomic loci. Bipolar disorder risk alleles were enriched in genes in synaptic signaling pathways and brain-expressed genes, particularly those with high specificity of expression in neurons of the prefrontal cortex and hippocampus. Significant signal enrichment was found in genes encoding targets of antipsychotics, calcium channel blockers, antiepileptics and anesthetics. Integrating expression quantitative trait locus data implicated 15 genes robustly linked to bipolar disorder via gene expression, encoding druggable targets such as HTR6, MCHR1, DCLK3 and FURIN. Analyses of bipolar disorder subtypes indicated high but imperfect genetic correlation between bipolar disorder type I and II and identified additional associated loci. Together, these results advance our understanding of the biological etiology of bipolar disorder, identify novel therapeutic leads and prioritize genes for functional follow-up studies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

The genetics of bipolar disorder
Independent replications and integrative analyses confirm TRANK1 as a susceptibility gene for bipolar disorder

Genetics of bipolar disorder: insights into its complex architecture and biology from common and rare variants
Data availability.
GWAS summary statistics are publicly available on the PGC website ( https://www.med.unc.edu/pgc/results-and-downloads ). Individual-level data are accessible through collaborative analysis proposals to the Bipolar Disorder Working Group of the PGC ( https://www.med.unc.edu/pgc/shared-methods/how-to/ ). This study included some publicly available datasets accessed through dbGaP (PGC bundle phs001254 ) and the HRC reference panel v1.0 ( http://www.haplotype-reference-consortium.org/home ). Databases used: Drug–Gene Interaction Database DGIdb v.2 ( https://www.dgidb.org ); Psychoactive Drug Screening Database Ki DB ( https://pdsp.unc.edu/databases/kidb.php ); DrugBank 5.0 ( https://www.drugbank.ca ); LD Hub ( http://ldsc.broadinstitute.org ); FUMA ( https://fuma.ctglab.nl ).
Code availability
All software used is publicly available at the URLs or references cited.
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390 , 1211–1259 (2017).
Article Google Scholar
Plans, L. et al. Association between completed suicide and bipolar disorder: a systematic review of the literature. J. Affect. Disord. 242 , 111–122 (2019).
Article CAS PubMed Google Scholar
American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association Publishing, 2013).
Merikangas, K. R. et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch. Gen. Psychiatry 64 , 543–552 (2007).
Article PubMed PubMed Central Google Scholar
Merikangas, K. R. et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch. Gen. Psychiatry 68 , 241–251 (2011).
Craddock, N. & Sklar, P. Genetics of bipolar disorder. Lancet 381 , 1654–1662 (2013).
Song, J. et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 17 , 184–193 (2015).
Article PubMed Google Scholar
Bienvenu, O. J., Davydow, D. S. & Kendler, K. S. Psychiatric ‘diseases’ versus behavioral disorders and degree of genetic influence. Psychol. Med. 41 , 33–40 (2011).
Psychiatric GWAS Consortium Bipolar Disorder Working Group. Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4 . Nat. Genet. 43 , 977–983 (2011).
Article CAS Google Scholar
Baum, A. E. et al. A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder. Mol. Psychiatry 13 , 197–207 (2008).
Charney, A. W. et al. Evidence for genetic heterogeneity between clinical subtypes of bipolar disorder. Transl. Psychiatry 7 , e993 (2017).
Article CAS PubMed PubMed Central Google Scholar
Chen, D. T. et al. Genome-wide association study meta-analysis of European and Asian-ancestry samples identifies three novel loci associated with bipolar disorder. Mol. Psychiatry 18 , 195–205 (2013).
Cichon, S. et al. Genome-wide association study identifies genetic variation in neurocan as a susceptibility factor for bipolar disorder. Am. J. Hum. Genet. 88 , 372–381 (2011).
Ferreira, M. A. R. et al. Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat. Genet. 40 , 1056–1058 (2008).
Green, E. K. et al. Association at SYNE1 in both bipolar disorder and recurrent major depression. Mol. Psychiatry 18 , 614–617 (2013).
Green, E. K. et al. Replication of bipolar disorder susceptibility alleles and identification of two novel genome-wide significant associations in a new bipolar disorder case–control sample. Mol. Psychiatry 18 , 1302–1307 (2013).
Hou, L. et al. Genome-wide association study of 40,000 individuals identifies two novel loci associated with bipolar disorder. Hum. Mol. Genet. 25 , 3383–3394 (2016).
Mühleisen, T. W. et al. Genome-wide association study reveals two new risk loci for bipolar disorder. Nat. Commun. 5 , 3339 (2014).
Article PubMed CAS Google Scholar
Schulze, T. G. et al. Two variants in Ankyrin 3 ( ANK3 ) are independent genetic risk factors for bipolar disorder. Mol. Psychiatry 14 , 487–491 (2009).
Scott, L. J. et al. Genome-wide association and meta-analysis of bipolar disorder in individuals of European ancestry. Proc. Natl Acad. Sci. USA 106 , 7501–7506 (2009).
Sklar, P. et al. Whole-genome association study of bipolar disorder. Mol. Psychiatry 13 , 558–569 (2008).
Smith, E. N. et al. Genome-wide association study of bipolar disorder in European American and African American individuals. Mol. Psychiatry 14 , 755–763 (2009).
Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447 , 661–678 (2007).
Stahl, E. A. et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat. Genet. 51 , 793–803 (2019).
Lee, S.-H., Zabolotny, J. M., Huang, H., Lee, H. & Kim, Y.-B. Insulin in the nervous system and the mind: functions in metabolism, memory, and mood. Mol. Metab. 5 , 589–601 (2016).
McIntyre, R. S. et al. A randomized, double-blind, controlled trial evaluating the effect of intranasal insulin on neurocognitive function in euthymic patients with bipolar disorder. Bipolar Disord. 14 , 697–706 (2012).
Nurnberger, J. I. Jr et al. Identification of pathways for bipolar disorder: a meta-analysis. JAMA Psychiatry 71 , 657–664 (2014).
Gordovez, F. J. A. & McMahon, F. J. The genetics of bipolar disorder. Mol. Psychiatry 25 , 544–559 (2020).
Zhang, C., Xiao, X., Li, T. & Li, M. Translational genomics and beyond in bipolar disorder. Mol. Psychiatry 26 , 186–202 (2021).
Pedersen, C. B. et al. The iPSYCH2012 case–cohort sample: new directions for unravelling genetic and environmental architectures of severe mental disorders. Mol. Psychiatry 1 , 6–14 (2018).
Gudbjartsson, D. F. et al. Large-scale whole-genome sequencing of the Icelandic population. Nat. Genet. 47 , 435–444 (2015).
Leitsalu, L. et al. Cohort Profile: Estonian Biobank of the Estonian Genome Center, University of Tartu. Int. J. Epidemiol. 44 , 1137–1147 (2015).
Krokstad, S. et al. Cohort Profile: the HUNT Study, Norway. Int. J. Epidemiol. 42 , 968–977 (2013).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12 , e1001779 (2015).
Bulik-Sullivan, B. K. et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47 , 291–295 (2015).
Loh, P.-R., Kichaev, G., Gazal, S., Schoech, A. P. & Price, A. L. Mixed-model association for biobank-scale datasets. Nat. Genet. 50 , 906–908 (2018).
de Leeuw, C. A., Mooij, J. M., Heskes, T. & Posthuma, D. MAGMA: generalized gene-set analysis of GWAS data. PLoS Comput. Biol. 11 , e1004219 (2015).
Article PubMed PubMed Central CAS Google Scholar
Bryois, J. et al. Genetic identification of cell types underlying brain complex traits yields insights into the etiology of Parkinson’s disease. Nat. Genet. 52 , 482–493 (2020).
Wagner, A. H. et al. DGIdb 2.0: mining clinically relevant drug–gene interactions. Nucleic Acids Res. 44 , D1036–D1044 (2016).
Roth, B. L., Lopez, E., Patel, S. & Kroeze, W. K. The multiplicity of serotonin receptors: uselessly diverse molecules or an embarrassment of riches? Neuroscientist 6 , 252–262 (2000).
Gaspar, H. A. & Breen, G. Drug enrichment and discovery from schizophrenia genome-wide association results: an analysis and visualisation approach. Sci. Rep. 7 , 12460 (2017).
Gusev, A. et al. Integrative approaches for large-scale transcriptome-wide association studies. Nat. Genet. 48 , 245–252 (2016).
Gandal, M. J. et al. Transcriptome-wide isoform-level dysregulation in ASD, schizophrenia, and bipolar disorder. Science 362 , eaat8127 (2018).
Mancuso, N. et al. Probabilistic fine-mapping of transcriptome-wide association studies. Nat. Genet. 51 , 675–682 (2019).
Zhu, Z. et al. Integration of summary data from GWAS and eQTL studies predicts complex trait gene targets. Nat. Genet. 48 , 481–487 (2016).
Wu, Y. et al. Integrative analysis of omics summary data reveals putative mechanisms underlying complex traits. Nat. Commun. 9 , 918 (2018).
Võsa, U. et al. Unraveling the polygenic architecture of complex traits using blood eQTL metaanalysis. Preprint at bioRxiv https://doi.org/10.1101/447367 (2018).
Zheng, J. et al. LD Hub: a centralized database and web interface to perform LD score regression that maximizes the potential of summary level GWAS data for SNP heritability and genetic correlation analysis. Bioinformatics 33 , 272–279 (2017).
Frei, O. et al. Bivariate causal mixture model quantifies polygenic overlap between complex traits beyond genetic correlation. Nat. Commun. 10 , 2417 (2019).
Holland, D. et al. Beyond SNP heritability: polygenicity and discoverability of phenotypes estimated with a univariate Gaussian mixture model. PLoS Genet. 16 , e1008612 (2020).
Zhu, Z. et al. Causal associations between risk factors and common diseases inferred from GWAS summary data. Nat. Commun. 9 , 224 (2018).
Steardo, L. Jr et al. Sleep disturbance in bipolar disorder: neuroglia and circadian rhythms. Front. Psychiatry 10 , 501 (2019).
Hunt, G. E., Malhi, G. S., Cleary, M., Lai, H. M. X. & Sitharthan, T. Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990–2015: systematic review and meta-analysis. J. Affect. Disord. 206 , 331–349 (2016).
Heffner, J. L., Strawn, J. R., DelBello, M. P., Strakowski, S. M. & Anthenelli, R. M. The co-occurrence of cigarette smoking and bipolar disorder: phenomenology and treatment considerations. Bipolar Disord. 13 , 439–453 (2011).
Vreeker, A. et al. High educational performance is a distinctive feature of bipolar disorder: a study on cognition in bipolar disorder, schizophrenia patients, relatives and controls. Psychol. Med. 46 , 807–818 (2016).
MacCabe, J. H. et al. Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. Br. J. Psychiatry 196 , 109–115 (2010).
Broome, M. R., Saunders, K. E. A., Harrison, P. J. & Marwaha, S. Mood instability: significance, definition and measurement. Br. J. Psychiatry 207 , 283–285 (2015).
Ward, J. et al. The genomic basis of mood instability: identification of 46 loci in 363,705 UK Biobank participants, genetic correlation with psychiatric disorders, and association with gene expression and function. Mol. Psychiatry 25 , 3091–3099 (2020).
Ikeda, M. et al. A genome-wide association study identifies two novel susceptibility loci and trans population polygenicity associated with bipolar disorder. Mol. Psychiatry 23 , 639–647 (2018).
Pardiñas, A. F. et al. Common schizophrenia alleles are enriched in mutation-intolerant genes and in regions under strong background selection. Nat. Genet. 50 , 381–389 (2018).
Howard, D. M. et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat. Neurosci. 22 , 343–352 (2019).
Smeland, O. B., Frei, O., Dale, A. M. & Andreassen, O. A. The polygenic architecture of schizophrenia – rethinking pathogenesis and nosology. Nat. Rev. Neurol. 16 , 366–379 (2020).
Sekar, A. et al. Schizophrenia risk from complex variation of complement component 4. Nature 530 , 177–183 (2016).
GTEx Consortium et al. Genetic effects on gene expression across human tissues. Nature 550 , 204–213 (2017).
Article PubMed Central Google Scholar
Brainstorm Consortium et al. Analysis of shared heritability in common disorders of the brain. Science 360 , eaap8757 (2018).
Cross-Disorder Group of the Psychiatric Genomics Consortium. Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell 179 , 1469–1482 (2019).
Article PubMed Central CAS Google Scholar
Lewis, K. J. S. et al. Comparison of genetic liability for sleep traits among individuals with bipolar disorder I or II and control participants. JAMA Psychiatry 77 , 303–310 (2020).
Zhou, H. et al. Genome-wide meta-analysis of problematic alcohol use in 435,563 individuals yields insights into biology and relationships with other traits. Nat. Neurosci. 23 , 809–818 (2020).
Okbay, A. et al. Genome-wide association study identifies 74 loci associated with educational attainment. Nature 533 , 539–542 (2016).
Vermeulen, J. M. et al. Smoking and the risk for bipolar disorder: evidence from a bidirectional Mendelian randomisation study. Br. J. Psychiatry 218 , 88–94 (2021).
Peyrot, W. J. et al. The association between lower educational attainment and depression owing to shared genetic effects? Results in ~25 000 subjects. Mol. Psychiatry 20 , 735–743 (2015).
Swanson, C. L. Jr, Gur, R. C., Bilker, W., Petty, R. G. & Gur, R. E. Premorbid educational attainment in schizophrenia: association with symptoms, functioning, and neurobehavioral measures. Biol. Psychiatry 44 , 739–747 (1998).
Wishart, D. S. et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 46 , D1074–D1082 (2018).
Mizuno, A. & Okada, Y. Biological characterization of expression quantitative trait loci (eQTLs) showing tissue-specific opposite directional effects. Eur. J. Hum. Genet. 27 , 1745–1756 (2019).
Schrode, N. et al. Synergistic effects of common schizophrenia risk variants. Nat. Genet. 51 , 1475–1485 (2019).
Jiang, X. et al. Sodium valproate rescues expression of TRANK1 in iPSC-derived neural cells that carry a genetic variant associated with serious mental illness. Mol. Psychiatry 24 , 613–624 (2019).
Huckins, L. M. et al. Transcriptomic imputation of bipolar disorder and bipolar subtypes reveals 29 novel associated genes. Preprint at bioRxiv https://doi.org/10.1101/222786 (2017).
Finan, C. et al. The druggable genome and support for target identification and validation in drug development. Sci. Transl. Med. 9 , eaag1166 (2017).
von Wegerer, J., Hesslinger, B., Berger, M. & Walden, J. A calcium antagonistic effect of the new antiepileptic drug lamotrigine. Eur. Neuropsychopharmacol. 7 , 77–81 (1997).
Cipriani, A. et al. A systematic review of calcium channel antagonists in bipolar disorder and some considerations for their future development. Mol. Psychiatry 21 , 1324–1332 (2016).
Harrison, P. J., Tunbridge, E. M., Dolphin, A. C. & Hall, J. Voltage-gated calcium channel blockers for psychiatric disorders: genomic reappraisal. Br. J. Psychiatry 216 , 250–253 (2020).
Network and Pathway Analysis Subgroup of Psychiatric Genomics Consortium. Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nat. Neurosci. 18 , 199–209 (2015).
Forstner, A. J. et al. Identification of shared risk loci and pathways for bipolar disorder and schizophrenia. PLoS ONE 12 , e0171595 (2017).
Bipolar Disorder and Schizophrenia Working Group of the Psychiatric Genomics Consortium. Genomic dissection of bipolar disorder and schizophrenia, including 28 subphenotypes. Cell 173 , 1705–1715 (2018).
Lee, Y., Zhang, Y., Kim, S. & Han, K. Excitatory and inhibitory synaptic dysfunction in mania: an emerging hypothesis from animal model studies. Exp. Mol. Med. 50 , 1–11 (2018).
PubMed PubMed Central Google Scholar
Skene, N. G. et al. Genetic identification of brain cell types underlying schizophrenia. Nat. Genet. 50 , 825–833 (2018).
Lewis, C. M. & Vassos, E. Polygenic risk scores: from research tools to clinical instruments. Genome Med. 12 , 44 (2020).
Torkamani, A., Wineinger, N. E. & Topol, E. J. The personal and clinical utility of polygenic risk scores. Nat. Rev. Genet. 19 , 581–590 (2018).
Duncan, L. et al. Analysis of polygenic risk score usage and performance in diverse human populations. Nat. Commun. 10 , 3328 (2019).
Martin, A. R. et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 51 , 584–591 (2019).
Coleman, J. R. I. et al. The genetics of the mood disorder spectrum: genome-wide association analyses of more than 185,000 cases and 439,000 controls. Biol. Psychiatry 88 , 169–184 (2020).
Moon, S. et al. The Korea Biobank Array: design and identification of coding variants associated with blood biochemical traits. Sci. Rep. 9 , 1382 (2019).
Bigdeli, T. B. et al. Contributions of common genetic variants to risk of schizophrenia among individuals of African and Latino ancestry. Mol. Psychiatry 25 , 2455–2467 (2020).
Lam, M. et al. RICOPILI: Rapid Imputation for COnsortias PIpeLIne. Bioinformatics 36 , 930–933 (2020).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38 , 904–909 (2006).
Loh, P.-R. et al. Reference-based phasing using the haplotype reference consortium panel. Nat. Genet. 48 , 1443–1448 (2016).
Das, S. et al. Next-generation genotype imputation service and methods. Nat. Genet. 48 , 1284–1287 (2016).
McCarthy, S. et al. A reference panel of 64,976 haplotypes for genotype imputation. Nat. Genet. 48 , 1279–1283 (2016).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4 , 7 (2015).
Willer, C. J., Li, Y. & Abecasis, G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26 , 2190–2191 (2010).
Demontis, D. et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat. Genet. 51 , 63–75 (2019).
Nievergelt, C. M. et al. International meta-analysis of PTSD genome-wide association studies identifies sex- and ancestry-specific genetic risk loci. Nat. Commun. 10 , 4558 (2019).
Purves, K. L. et al. A major role for common genetic variation in anxiety disorders. Mol. Psychiatry 25 , 3292–3303 (2020).
Yu, D. et al. Interrogating the genetic determinants of Tourette’s syndrome and other tic disorders through genome-wide association studies. Am. J. Psychiatry 176 , 217–227 (2019).
Watson, H. J. et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat. Genet. 51 , 1207–1214 (2019).
Grove, J. et al. Identification of common genetic risk variants for autism spectrum disorder. Nat. Genet. 51 , 431–444 (2019).
Quinlan, A. R. & Hall, I. M. BEDTools: a flexible suite of utilities for comparing genomic features. Bioinformatics 26 , 841–842 (2010).
Watanabe, K., Taskesen, E., van Bochoven, A. & Posthuma, D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 8 , 1826 (2017).
Zeisel, A. et al. Molecular architecture of the mouse nervous system. Cell 174 , 999–1014 (2018).
Saunders, A. et al. Molecular diversity and specializations among the cells of the adult mouse brain. Cell 174 , 1015–1030 (2018).
Habib, N. et al. Massively parallel single-nucleus RNA-seq with DroNc-seq. Nat. Methods 14 , 955–958 (2017).
Lake, B. B. et al. Integrative single-cell analysis of transcriptional and epigenetic states in the human adult brain. Nat. Biotechnol. 36 , 70–80 (2018).
1000 Genomes Project Consortium. et al. A global reference for human genetic variation. Nature 526 , 68–74 (2015).
Kamitaki, N. et al. Complement genes contribute sex-biased vulnerability in diverse disorders. Nature 582 , 577–581 (2020).
Browning, S. R. & Browning, B. L. Rapid and accurate haplotype phasing and missing-data inference for whole-genome association studies by use of localized haplotype clustering. Am. J. Hum. Genet. 81 , 1084–1097 (2007).
Browning, B. L. & Browning, S. R. Genotype imputation with millions of reference samples. Am. J. Hum. Genet. 98 , 116–126 (2016).
Lee, S. H., Goddard, M. E., Wray, N. R. & Visscher, P. M. A better coefficient of determination for genetic profile analysis. Genet. Epidemiol. 36 , 214–224 (2012).
Hemani, G., Tilling, K. & Davey Smith, G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 13 , e1007081 (2017).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife 7 , e34408 (2018).
Verbanck, M., Chen, C.-Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50 , 693–698 (2018).
Hübel, C. et al. Genomics of body fat percentage may contribute to sex bias in anorexia nervosa. Am. J. Med. Genet. B Neuropsychiatr. Genet. 180 , 428–438 (2019).
Download references
Acknowledgements
We thank the participants who donated their time, life experiences and DNA to this research and the clinical and scientific teams that worked with them. We are deeply indebted to the investigators who make up the PGC. The PGC has received major funding from the US National Institute of Mental Health (PGC3: U01 MH109528; PGC2: U01 MH094421; PGC1: U01 MH085520). Statistical analyses were carried out on the NL Genetic Cluster Computer ( http://www.geneticcluster.org ) hosted by SURFsara and the Mount Sinai high-performance computing cluster ( http://hpc.mssm.edu ), which is supported by the Office of Research Infrastructure of the National Institutes of Health under award numbers S10OD018522 and S10OD026880. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Full acknowledgements are included in the Supplementary Note .
Author information
These authors contributed equally: Niamh Mullins, Andreas J. Forstner.
These authors jointly supervised this work: Eli A. Stahl, Andrew McQuillin, Arianna Di Florio, Roel A. Ophoff, Ole A. Andreassen.
A list of members and their affiliations appears in the Supplementary Information.
Authors and Affiliations
Department of Genetics and Genomic Sciences, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Niamh Mullins, Brian M. Schilder, Laura G. Sloofman, Amanda L. Dobbyn, Laura Huckins, Jessica S. Johnson, Dolores Malaspina, Towfique Raj, Panos Roussos, Hannah Young & Eli A. Stahl
Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Niamh Mullins, Alexander W. Charney, Amanda L. Dobbyn, Laura Huckins, Jessica S. Johnson, Dolores Malaspina, Panos Roussos, René S. Kahn & Eli A. Stahl
Institute of Human Genetics, University of Bonn, School of Medicine and University Hospital Bonn, Bonn, Germany
Andreas J. Forstner, Eva C. Beins, Friederike S. David, Franziska Degenhardt, Stefan Herms, Per Hoffmann, Markus M. Nöthen & Sven Cichon
Institute of Neuroscience and Medicine (INM-1), Research Centre Jülich, Jülich, Germany
Andreas J. Forstner, Thomas W. Mühleisen & Sven Cichon
Centre for Human Genetics, University of Marburg, Marburg, Germany
Andreas J. Forstner
Division of Mental Health and Addiction, Oslo University Hospital, Oslo, Norway
Kevin S. O’Connell, Oleksandr Frei, Olav B. Smeland, Ingrid Melle & Ole A. Andreassen
NORMENT, University of Oslo, Oslo, Norway
Kevin S. O’Connell, Olav B. Smeland & Ole A. Andreassen
Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA
Brandon Coombes & Joanna M. Biernacka
Social, Genetic and Developmental Psychiatry Centre, King’s College London, London, UK
Jonathan R. I. Coleman, Saskia P. Hagenaars, Peter McGuffin, Gerome Breen, Panagiotis Ferentinos & Cathryn M. Lewis
NIHR Maudsley BRC, King’s College London, London, UK
Jonathan R. I. Coleman, Saskia P. Hagenaars, Gerome Breen & Cathryn M. Lewis
Institute for Molecular Bioscience, The University of Queensland, Brisbane, Queensland, Australia
Zhen Qiao, Grant W. Montgomery & Naomi R. Wray
iSEQ, Center for Integrative Sequencing, Aarhus University, Aarhus, Denmark
Thomas D. Als, Jakob Grove, Manuel Mattheisen & Preben Bo Mortensen
Department of Biomedicine - Human Genetics, Aarhus University, Aarhus, Denmark
Thomas D. Als, Jakob Grove & Manuel Mattheisen
iPSYCH, The Lundbeck Foundation Initiative for Integrative Psychiatric Research, Aarhus, Denmark
Thomas D. Als, Esben Agerbo, Marie Bækvad-Hansen, Carsten Bøcker Pedersen, Jonas Bybjerg-Grauholm, Marianne Giørtz Pedersen, Jakob Grove, Manuel Mattheisen, Christine Søholm Hansen, Anders D. Børglum, David M. Hougaard, Ole Mors, Preben Bo Mortensen, Merete Nordentoft & Thomas Werge
Department of Psychiatry and Behavioral Sciences, SUNY Downstate Health Sciences University, Brooklyn, NY, USA
Tim B. Bigdeli
VA NY Harbor Healthcare System, Brooklyn, NY, USA
Research and Communication Unit for Musculoskeletal Health, Division of Clinical Neuroscience, Oslo University Hospital, Oslo, Norway
Sigrid Børte
Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Sigrid Børte, Torbjørn Elvsåshagen, Oleksandr Frei & John-Anker Zwart
K. G. Jebsen Center for Genetic Epidemiology, Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway
Sigrid Børte, Bendik S. Winsvold, Ben M. Brumpton, Kristian Hveem & John-Anker Zwart
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Julien Bryois, Sarah E. Bergen, Dennis Hellgren, Christina M. Hultman, Mikael Landén & Patrick F. Sullivan
Department of Mental Health, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology (NTNU), Trondheim, Norway
Ole Kristian Drange & Gunnar Morken
Department of Østmarka, Division of Mental Health Care, St Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
Ole Kristian Drange
Department of Psychiatry and Biobehavioral Science, Semel Institute, David Geffen School of Medicine, University of California, Los Angeles, Los Angeles, CA, USA
Michael J. Gandal, Minsoo Kim, Nelson B. Freimer, Loes M. Olde Loohuis & Roel A. Ophoff
Department of Psychiatry, School of Medicine, Fujita Health University, Toyoake, Japan
Masashi Ikeda, Nakao Iwata & Takeo Saito
Stanley Center for Psychiatric Research, Broad Institute, Cambridge, MA, USA
Nolan Kamitaki, Steven A. McCarroll, Jennifer L. Moran, Benjamin M. Neale, Stephan Ripke & Jordan W. Smoller
Department of Genetics, Harvard Medical School, Boston, MA, USA
Nolan Kamitaki, Steven A. McCarroll & Tõnu Esko
Estonian Genome Center, Institute of Genomics, University of Tartu, Tartu, Estonia
Kristi Krebs, Tõnu Esko & Lili Milani
Department of Psychiatry and Psychotherapy, Charité - Universitätsmedizin, Berlin, Germany
Georgia Panagiotaropoulou, Vassily Trubetskoy, Swapnil Awasthi & Stephan Ripke
Department of Neuroscience, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Brian M. Schilder, Towfique Raj & Panos Roussos
Ronald M. Loeb Center for Alzheimer’s Disease, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Brian M. Schilder & Towfique Raj
Estelle and Daniel Maggin Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
deCODE Genetics/Amgen, Reykjavik, Iceland
Stacy Steinberg, Sigurdur H. Magnusson, Thorgeir E. Thorgeirsson, Hreinn Stefansson & Kari Stefansson
Department of Research, Innovation and Education, Division of Clinical Neuroscience, Oslo University Hospital, Oslo, Norway
Bendik S. Winsvold & John-Anker Zwart
Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea
Hong-Hee Won
Russian Academy of Medical Sciences, Mental Health Research Center, Moscow, Russian Federation
Liliya Abramova
Institute of Psychiatric Phenomics and Genomics (IPPG), University Hospital, LMU Munich, Munich, Germany
Kristina Adorjan, Monika Budde, Katrin Gade, Urs Heilbronner, Janos L. Kalman, Sergi Papiol, Eva C. Schulte, Fanny Senner & Thomas G. Schulze
Department of Psychiatry and Psychotherapy, University Hospital, LMU Munich, Munich, Germany
Kristina Adorjan, Janos L. Kalman, Sergi Papiol, Eva C. Schulte & Fanny Senner
National Centre for Register-Based Research, Aarhus University, Aarhus, Denmark
Esben Agerbo, Carsten Bøcker Pedersen, Marianne Giørtz Pedersen & Preben Bo Mortensen
Centre for Integrated Register-Based Research, Aarhus University, Aarhus, Denmark
Division of Psychiatry, University College London, London, UK
Mariam Al Eissa, Nicholas Bass, Alessia Fiorentino, Niamh O’Brien, Sally Sharp & Andrew McQuillin
Department of Neuroscience, Istituto Di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy
Diego Albani
Department of Psychiatry and Behavioral Neuroscience, University of Chicago, Chicago, IL, USA
Ney Alliey-Rodriguez & Elliot S. Gershon
Northwestern University, Chicago, IL, USA
Ney Alliey-Rodriguez
Psychiatry, Berkshire Healthcare NHS Foundation Trust, Bracknell, UK
Adebayo Anjorin
Analytic and Translational Genetics Unit, Massachusetts General Hospital, Boston, MA, USA
Verneri Antilla, Benjamin M. Neale & Stephan Ripke
2nd Department of Psychiatry, Attikon General Hospital, National and Kapodistrian University of Athens, Athens, Greece
Anastasia Antoniou, Athanassios Douzenis, Evgenia Porichi & Panagiotis Ferentinos
Department of Psychiatry, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, South Korea
Ji Hyun Baek & Kyung Sue Hong
Center for Neonatal Screening, Department for Congenital Disorders, Statens Serum Institut, Copenhagen, Denmark
Marie Bækvad-Hansen, Jonas Bybjerg-Grauholm, Christine Søholm Hansen & David M. Hougaard
Department of Psychiatry and Psychotherapy, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
Michael Bauer & Andrea Pfennig
Department of Psychiatry and Psychotherapeutic Medicine, Medical University of Graz, Graz, Austria
Armin Birner, Nina Dalkner, Susanne Bengesser & Eva Z. Reininghaus
Department of Psychiatric Research, Diakonhjemmet Hospital, Oslo, Norway
Erlend Bøen & Ingrid Agartz
Psychiatry, Brain Center UMC Utrecht, Utrecht, the Netherlands
Marco P. Boks & René S. Kahn
Instituto de Salud Carlos III, Biomedical Network Research Centre on Mental Health (CIBERSAM), Madrid, Spain
Rosa Bosch, Miquel Casas, Cristina Sánchez-Mora, Maria Soler Artigas, Josep Antoni Ramos-Quiroga & Marta Ribasés
Department of Psychiatry, Hospital Universitari Vall d´Hebron, Barcelona, Spain
Department of Psychiatry and Forensic Medicine, Universitat Autònoma de Barcelona, Barcelona, Spain
Rosa Bosch, Miquel Casas & Josep Antoni Ramos-Quiroga
Psychiatric Genetics Unit, Group of Psychiatry Mental Health and Addictions, Vall d´Hebron Research Institut (VHIR), Universitat Autònoma de Barcelona, Barcelona, Spain
Department of Psychiatry, Psychosomatic Medicine and Psychotherapy, University Hospital Frankfurt, Frankfurt am Main, Germany
Murielle Brum, Nathalie Brunkhorst-Kanaan, Sarah Kittel-Schneider, Thorsten M. Kranz & Andreas Reif
Psychiatry, University of California San Francisco, San Francisco, CA, USA
William Byerley
University of Newcastle, Newcastle, New South Wales, Australia
Murray Cairns, Paul Tooney, Frans Henskens, Carmel Loughland, Patricia Michie, Ulrich Schall & Rodney J. Scott
Mood Disorders Program, Department of Psychiatry, McGill University Health Center, Montreal, Quebec, Canada
Pablo Cervantes & Cristiana Cruceanu
Division of Psychiatry, University of Edinburgh, Edinburgh, UK
Toni-Kim Clarke & Douglas H. R. Blackwood
Department of Translational Research in Psychiatry, Max Planck Institute of Psychiatry, Munich, Germany
Cristiana Cruceanu, Susanne Lucae & Bertram Müller-Myhsok
Department of Psychiatry, Universidad Autonoma de Nuevo Leon, Monterrey, Mexico
Alfredo Cuellar-Barboza
Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN, USA
Alfredo Cuellar-Barboza, Mark Frye & Joanna M. Biernacka
Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, USA
Julie Cunningham
Centre for Psychiatry, Queen Mary University of London, London, UK
David Curtis
UCL Genetics Institute, University College London, London, UK
Department of Psychiatry, Laboratory of Psychiatric Genetics, Poznan University of Medical Sciences, Poznan, Poland
Piotr M. Czerski & Joanna Hauser
Center for Multimodal Imaging and Genetics, Departments of Neurosciences, Radiology, and Psychiatry, University of California, San Diego, CA, USA
Anders M. Dale
Department of Child and Adolescent Psychiatry, Psychosomatics and Psychotherapy, University Hospital Essen, University of Duisburg-Essen, Duisburg, Germany
Franziska Degenhardt
Department of Medical Genetics, Oslo University Hospital, Oslo, Norway
Srdjan Djurovic
NORMENT, Department of Clinical Science, University of Bergen, Bergen, Norway
Department of Neurology, Oslo University Hospital, Oslo, Norway
Torbjørn Elvsåshagen
NORMENT, KG Jebsen Centre for Psychosis Research, Oslo University Hospital, Oslo, Norway
Medical Research Council Centre for Neuropsychiatric Genetics and Genomics, Division of Psychological Medicine and Clinical Neurosciences, Cardiff University, Cardiff, UK
Valentina Escott-Price, Liz Forty, Peter A. Holmans, Catrin Lewis, Antonio F. Pardiñas, James T. R. Walters, Jessica Mei Kay Yang, Nicholas Craddock, Ian Jones, George Kirov, Michael C. O’Donovan, Michael J. Owen & Arianna Di Florio
Academic Psychiatry, Newcastle University, Newcastle upon Tyne, UK
I. Nicol Ferrier
Department of Medical and Molecular Genetics, Indiana University, Indianapolis, IN, USA
Tatiana M. Foroud & Howard J. Edenberg
Department of Genetic Epidemiology in Psychiatry, Central Institute of Mental Health, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany
Josef Frank, Lea Sirignano, Stephanie H. Witt, Lea Zillich, Marcella Rietschel, Thomas G. Schulze & Fabian Streit
Center for Neurobehavioral Genetics, Semel Institute for Neuroscience and Human Behavior, Los Angeles, CA, USA
Nelson B. Freimer, Loes M. Olde Loohuis & Roel A. Ophoff
Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
Louise Frisén, Lina Martinsson & Jan Hillert
Department of Psychiatry and Psychotherapy, University Medical Center Göttingen, Göttingen, Germany
Katrin Gade & Thomas G. Schulze
Department of Psychiatry, Dalhousie University, Halifax, Nova Scotia, Canada
Julie Garnham, Claire O’Donovan, Claire Slaney & Martin Alda
Department of Psychiatry, Yale School of Medicine, New Haven, CT, USA
Joel Gelernter & Hang Zhou
Veterans Affairs Connecticut Healthcare System, West Haven, CT, USA
Departments of Genetics and Neuroscience, Yale University School of Medicine, New Haven, CT, USA
Joel Gelernter
Department of Psychological Sciences, University of Missouri, Columbia, MO, USA
Ian R. Gizer
Genetics and Computational Biology, QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia
Scott D. Gordon, Sarah E. Medland & Nicholas G. Martin
Psychological Medicine, University of Worcester, Worcester, UK
Katherine Gordon-Smith, Amy Perry & Lisa A. Jones
Department of Psychiatry, University of California San Diego, La Jolla, CA, USA
Tiffany A. Greenwood, Adam Maihofer, Paul D. Shilling, John R. Kelsoe & Caroline M. Nievergelt
Bioinformatics Research Centre, Aarhus University, Aarhus, Denmark
Jakob Grove
Mental Health Department, University Regional Hospital, Biomedicine Institute (IBIMA), Málaga, Spain
José Guzman-Parra, Fabio Rivas & Fermin Mayoral
Department of Psychiatry, Seoul National University College of Medicine, Seoul, South Korea
Kyooseob Ha
Landspitali University Hospital, Reykjavik, Iceland
Magnus Haraldsson & Engilbert Sigurdsson
Department of Psychology, Eberhard Karls Universität Tübingen, Tübingen, Germany
Martin Hautzinger
Department of Biomedicine, University of Basel, Basel, Switzerland
Stefan Herms, Per Hoffmann, Thomas W. Mühleisen & Sven Cichon
Institute of Medical Genetics and Pathology, University Hospital Basel, Basel, Switzerland
Stefan Herms, Per Hoffmann & Sven Cichon
Neuropsychiatrie Translationnelle, Inserm U955, Créteil, France
Stéphane Jamain & Marion Leboyer
Faculté de Santé, Université Paris Est, Créteil, France
International Max Planck Research School for Translational Psychiatry (IMPRS-TP), Munich, Germany
Janos L. Kalman
Laboratory of Complex Trait Genomics, Department of Computational Biology and Medical Sciences, Graduate School of Frontier Sciences, The University of Tokyo, Tokyo, Japan
Yoichiro Kamatani
Laboratory for Statistical and Translational Genetics, RIKEN Center for Integrative Medical Sciences, Yokohama, Japan
Yoichiro Kamatani & Chikashi Terao
Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
James L. Kennedy, John S. Strauss & John B. Vincent
Neurogenetics Section, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
James L. Kennedy
Department of Psychiatry, University of Toronto, Toronto, Ontario, Canada
Institute of Medical Sciences, University of Toronto, Toronto, Ontario, Canada
Department of Psychiatry, Psychosomatics and Psychotherapy, Center of Mental Health, University Hospital Würzburg, Würzburg, Germany
Sarah Kittel-Schneider, Manuel Mattheisen, Julian Roth & Micha Gawlik
Cell Biology, SUNY Downstate Medical Center College of Medicine, Brooklyn, NY, USA
James A. Knowles
Institute for Genomic Health, SUNY Downstate Medical Center College of Medicine, Brooklyn, NY, USA
James A. Knowles, Helena Medeiros, Carlos Pato & Michele T. Pato
ISGlobal, Barcelona, Spain
Manolis Kogevinas
Laboratory of Pharmacogenomics and Individualized Therapy, Department of Pharmacy, School of Health Sciences, University of Patras, Patras, Greece
Maria Koromina, Evangelia-Eirini Tsermpini & George P. Patrinos
Mental Illness Research, Education and Clinical Center, Crescenz VAMC, Philadelphia, PA, USA
Henry R. Kranzler
Center for Studies of Addiction, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA
RIKEN Center for Integrative Medical Sciences, Yokohama, Japan
Michiaki Kubo
Psychiatry, Altrecht, Utrecht, the Netherlands
Ralph Kupka
Psychiatry, GGZ inGeest, Amsterdam, the Netherlands
Psychiatry, VU Medisch Centrum, Amsterdam, the Netherlands
Department of Psychiatry, Erasmus MC, University Medical Center Rotterdam, Rotterdam, the Netherlands
Steven A. Kushner & Roel A. Ophoff
Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm, Sweden
Catharina Lavebratt, Martin Lundberg, Vincent Millischer, Lena Backlund & Martin Schalling
Center for Molecular Medicine, Karolinska University Hospital, Stockholm, Sweden
Psychiatry, North East London NHS Foundation Trust, Ilford, UK
Jacob Lawrence
Clinic for Psychiatry and Psychotherapy, University Hospital Cologne, Cologne, Germany
Markus Leber
Department of Psychiatry, Korea University College of Medicine, Seoul, South Korea
Heon-Jeong Lee
Psychiatric and Neurodevelopmental Genetics Unit, Center for Genomic Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA
Phil H. Lee
HudsonAlpha Institute for Biotechnology, Huntsville, AL, USA
Shawn E. Levy & Richard M. Myers
Department of Human Genetics, McGill University, Montréal, Quebec, Canada
Calwing Liao
Montreal Neurological Institute and Hospital, McGill University, Montréal, Quebec, Canada
Calwing Liao & Guy A. Rouleau
Division of Psychiatry, Centre for Clinical Brain Sciences, The University of Edinburgh, Edinburgh, UK
Donald J. MacIntyre & Andrew M. McIntosh
Department of Psychiatry and Psychotherapy, University of Bonn, Bonn, Germany
Wolfgang Maier
Clinical Biochemistry Laboratory, Attikon General Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece
Eirini Maratou
Department of Clinical Neuroscience, Centre for Psychiatry Research, Karolinska Institutet, Stockholm, Sweden
Manuel Mattheisen & Ingrid Agartz
Systems Genetics Working Group, Department of Genetics, Stellenbosch University, Stellenbosch, South Africa
Nathaniel W. McGregor
Genetic Cancer Susceptibility Group, International Agency for Research on Cancer, Lyon, France
James D. McKay
Department of Psychiatry, Massachusetts General Hospital, Boston, MA, USA
Jennifer L. Moran & Jordan W. Smoller
Centre for Neuroimaging and Cognitive Genomics (NICOG), National University of Ireland Galway, Galway, Ireland
Derek W. Morris
Medical Faculty, School of Science and Technology, University Sarajevo, Sarajevo, Bosnia and Herzegovina
Lilijana Oruc
Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, MD, USA
James B. Potash, J. Raymond DePaulo, Peter P. Zandi, Fernando S. Goes & Thomas G. Schulze
Oxford Health NHS Foundation Trust, Warneford Hospital, Oxford, UK
Digby Quested
Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, UK
Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA, USA
Mark H. Rapaport
Outpatient Clinic for Bipolar Disorder, Altrecht, Utrecht, the Netherlands
Eline J. Regeer
Department of Psychiatry, Washington University in Saint Louis, Saint Louis, MO, USA
John P. Rice
Department of Biochemistry and Molecular Biology II, Faculty of Pharmacy, University of Granada, Granada, Spain
Margarita Rivera
Institute of Neurosciences, Biomedical Research Center (CIBM), University of Granada, Granada, Spain
Medicine, Psychiatry, Biomedical Informatics, Vanderbilt University Medical Center, Nashville, TN, USA
Douglas M. Ruderfer
Department of Genetics, Microbiology and Statistics, Faculty of Biology, Universitat de Barcelona, Barcelona, Spain
Cristina Sánchez-Mora, Maria Soler Artigas & Marta Ribasés
Faculty of Medicine, Department of Psychiatry, School of Health Sciences, University of Iceland, Reykjavik, Iceland
Engilbert Sigurdsson
Institute of Health and Wellbeing, University of Glasgow, Glasgow, UK
Daniel J. Smith
Psychiatry and the Behavioral Sciences, University of Southern California, Los Angeles, CA, USA
Janet L. Sobell
Mood Disorders, PsyQ, Rotterdam, the Netherlands
Anne T. Spijker
SAMRC Unit on Risk and Resilience in Mental Disorders, Department of Psychiatry and Neuroscience Institute, University of Cape Town, Cape Town, South Africa
Dan J. Stein
Department of Environmental Epidemiology, Nofer Institute of Occupational Medicine, Lodz, Poland
Beata Świątkowska
Neuroscience Research Australia, Sydney, New South Wales, Australia
Claudio Toma, Janice M. Fullerton, Melissa J. Green, Peter R. Schofield, Cynthia Shannon Weickert & Thomas W. Weickert
School of Medical Sciences, University of New South Wales, Sydney, New South Wales, Australia
Claudio Toma, Janice M. Fullerton & Peter R. Schofield
Centro de Biología Molecular Severo Ochoa, Universidad Autónoma de Madrid and CSIC, Madrid, Spain
Claudio Toma
Department of Psychiatry and Human Behavior, School of Medicine, University of California, Irvine, Irvine, CA, USA
Marquis P. Vawter
Psychiatry, Psychiatrisches Zentrum Nordbaden, Wiesloch, Germany
Helmut Vedder
Computational Sciences Center of Emphasis, Pfizer Global Research and Development, Cambridge, MA, USA
Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada
Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Allan H. Young
South London and Maudsley NHS Foundation Trust, Bethlem Royal Hospital, Beckenham, UK
Department of Clinical Sciences, Psychiatry, Umeå University Medical Faculty, Umeå, Sweden
Rolf Adolfsson
NORMENT, KG Jebsen Centre for Psychosis Research, Division of Mental Health and Addiction, Institute of Clinical Medicine and Diakonhjemmet Hospital, University of Oslo, Oslo, Norway
Ingrid Agartz
National Institute of Mental Health, Klecany, Czech Republic
Martin Alda
Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden
Lars Alfredsson
Institute of Pulmonology, Russian State Medical University, Moscow, Russian Federation
Gulja Babadjanova
Department of Psychiatry, University of Münster, Münster, Germany
Bernhard T. Baune & Udo Dannlowski
Department of Psychiatry, Melbourne Medical School, The University of Melbourne, Melbourne, Victoria, Australia
Bernhard T. Baune
The Florey Institute of Neuroscience and Mental Health, The University of Melbourne, Parkville, Victoria, Australia
Université de Paris, INSERM, Optimisation Thérapeutique en Neuropsychopharmacologie, UMRS 1144, Paris, France
Frank Bellivier & Bruno Etain
APHP Nord, DMU Neurosciences, Département de Psychiatrie et de Médecine Addictologique, GHU Saint Louis-Lariboisière-Fernand Widal, Paris, France
Psychiatry, University of Pennsylvania, Philadelphia, PA, USA
Wade H. Berrettini
Center for Statistical Genetics and Department of Biostatistics, University of Michigan, Ann Arbor, MI, USA
Michael Boehnke & Laura J. Scott
Department of Biomedicine and the iSEQ Center, Aarhus University, Aarhus, Denmark
Anders D. Børglum
Center for Genomics and Personalized Medicine, CGPM, Aarhus, Denmark
School of Psychiatry, University of New South Wales, Sydney, New South Wales, Australia
Vaughan J. Carr, Melissa J. Green, Philip B. Mitchell, Cynthia Shannon Weickert & Thomas W. Weickert
University of Queensland, Brisbane, Queensland, Australia
Stanley Catts & Bryan Mowry
Neuropsychiatric Genetics Research Group, Department of Psychiatry and Trinity Translational Medicine Institute, Trinity College Dublin, Dublin, Ireland
Aiden Corvin
1st Department of Psychiatry, Eginition Hospital, National and Kapodistrian University of Athens, Athens, Greece
Dimitris Dikeos
Medical and Population Genetics, Broad Institute, Cambridge, MA, USA
Tõnu Esko, Benjamin M. Neale & Eli A. Stahl
Division of Endocrinology, Children’s Hospital Boston, Boston, MA, USA
Department of Human Genetics, University of Chicago, Chicago, IL, USA
Elliot S. Gershon
Biometric Psychiatric Genetics Research Unit, Alexandru Obregia Clinical Psychiatric Hospital, Bucharest, Romania
Maria Grigoroiu-Serbanescu
HUNT Research Center, Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway
Kristian Hveem
University of Western Australia, Nedlands, Western Australia, Australia
Assen V. Jablensky
Institute of Neuroscience and Physiology, University of Gothenburg, Gothenburg, Sweden
Mikael Landén
Department of Psychiatry and Addiction Medicine, Assistance Publique - Hôpitaux de Paris, Paris, France
Marion Leboyer
Department of Medical and Molecular Genetics, King’s College London, London, UK
Cathryn M. Lewis
Neuroscience Therapeutic Area, Janssen Research and Development, LLC, Titusville, NJ, USA
Qingqin S. Li
Cancer Epidemiology and Prevention, M. Sklodowska-Curie National Research Institute of Oncology, Warsaw, Poland
Jolanta Lissowska
SA MRC Unit on Risk and Resilience in Mental Disorders, Department of Psychiatry, Stellenbosch University, Stellenbosch, South Africa
Christine Lochner
School of Psychology, The University of Queensland, Brisbane, Queensland, Australia
Nicholas G. Martin
Department of Psychiatry and Genetics Institute, University of Florida, Gainesville, FL, USA
Carol A. Mathews
Research Institute, Lindner Center of HOPE, Mason, OH, USA
Susan L. McElroy
Centre for Cognitive Ageing and Cognitive Epidemiology, University of Edinburgh, Edinburgh, UK
Andrew M. McIntosh
Human Genetics Branch, Intramural Research Program, National Institute of Mental Health, Bethesda, MD, USA
Francis J. McMahon
Division of Mental Health and Addiction, University of Oslo, Institute of Clinical Medicine, Oslo, Norway
Ingrid Melle
Psychiatry, St Olavs University Hospital, Trondheim, Norway
Gunnar Morken
Psychosis Research Unit, Aarhus University Hospital - Psychiatry, Risskov, Denmark
Munich Cluster for Systems Neurology (SyNergy), Munich, Germany
Bertram Müller-Myhsok
University of Liverpool, Liverpool, UK
Research/Psychiatry, Veterans Affairs San Diego Healthcare System, San Diego, CA, USA
Caroline M. Nievergelt
Mental Health Services in the Capital Region of Denmark, Mental Health Center Copenhagen, University of Copenhagen, Copenhagen, Denmark
Merete Nordentoft
Division of Psychiatry, Haukeland Universitetssjukehus, Bergen, Norway
Ketil J. Oedegaard
Faculty of Medicine and Dentistry, University of Bergen, Bergen, Norway
Department of Clinical Neuroscience and Center for Molecular Medicine, Karolinska Institutet at Karolinska University Hospital, Solna, Sweden
Tomas Olsson
Human Genetics and Computational Biomedicine, Pfizer Global Research and Development, Groton, CT, USA
Sara A. Paciga
University of Melbourne, Melbourne, Victoria, Australia
Chris Pantelis
Department of Pathology, College of Medicine and Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates
George P. Patrinos
Zayed Center of Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates
Psychiatry, Harvard Medical School, Boston, MA, USA
Roy H. Perlis
Division of Clinical Research, Massachusetts General Hospital, Boston, MA, USA
Department of Complex Trait Genetics, Center for Neurogenomics and Cognitive Research, Amsterdam Neuroscience, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands
Danielle Posthuma
Department of Clinical Genetics, Amsterdam Neuroscience, Vrije Universiteit Medical Center, Amsterdam, the Netherlands
Department of Neurology and Neurosurgery, Faculty of Medicine, McGill University, Montreal, Quebec, Canada
Guy A. Rouleau
Department of Psychiatry and Behavioral Sciences, SUNY Upstate Medical University, Syracuse, NY, USA
Thomas G. Schulze
Department of Biomedical and NeuroMotor Sciences, University of Bologna, Bologna, Italy
Alessandro Serretti
Department of Neuroscience, SUNY Upstate Medical University, Syracuse, NY, USA
Cynthia Shannon Weickert & Thomas W. Weickert
Psychiatric and Neurodevelopmental Genetics Unit (PNGU), Massachusetts General Hospital, Boston, MA, USA
Jordan W. Smoller
Faculty of Medicine, University of Iceland, Reykjavik, Iceland
Kari Stefansson
Department of Psychiatry, Hospital Namsos, Namsos, Norway
Eystein Stordal
Department of Neuroscience, Norges Teknisk Naturvitenskapelige Universitet Fakultet for Naturvitenskap og Teknologi, Trondheim, Norway
Department of Genetics, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Patrick F. Sullivan
Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Patrick F. Sullivan & Arianna Di Florio
Department of Psychiatry, McGill University, Montreal, Quebec, Canada
Gustavo Turecki
Department of Psychiatry, Sankt Olavs Hospital Universitetssykehuset i Trondheim, Trondheim, Norway
Arne E. Vaaler
Clinical Institute of Neuroscience, Hospital Clinic, University of Barcelona, IDIBAPS, CIBERSAM, Barcelona, Spain
Eduard Vieta
Department of Psychology, Emory University, Atlanta, GA, USA
Irwin D. Waldman
Institute of Biological Psychiatry, Mental Health Services, Copenhagen University Hospital, Copenhagen, Denmark
Thomas Werge
Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Center for GeoGenetics, GLOBE Institute, University of Copenhagen, Copenhagen, Denmark
Queensland Brain Institute, The University of Queensland, Brisbane, Queensland, Australia
Naomi R. Wray
Psychiatry, Indiana University School of Medicine, Indianapolis, IN, USA
John I. Nurnberger
Biochemistry and Molecular Biology, Indiana University School of Medicine, Indianapolis, IN, USA
Howard J. Edenberg
Department of Human Genetics, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, CA, USA
Roel A. Ophoff
You can also search for this author in PubMed Google Scholar
HUNT All-In Psychiatry
- Bendik S. Winsvold
- , Eystein Stordal
- , Gunnar Morken
- , John-Anker Zwart
- , Ole Kristian Drange
- & Sigrid Børte
Contributions
Writing group: N.M., A.J.F., K.S.O’C., B.C., J.R.I.C., J.M.B., J.I.N., S. Cichon, H.J.E., E.A.S., A. McQuillin, A.D.F., R.A.O., O.A.A. PGC BD PI group: A.J.F., M.I., H.-H.W., D.C., R.A., I.A., M.A., L. Alfredsson, G. Babadjanova, L.B., B.T.B., F.B., S. Bengesser, W.H.B., D.H.R.B., M. Boehnke, A.D.B., G. Breen, V.J.C., S. Catts, A.C., N.C., U.D., D.D., T. Esko, B.E., P.F., M.F., J.M.F., M.G., E.S.G., F.S.G., M. J. Green, M.G.-S., J. Hauser, F.H., J. Hillert, K.S.H., D.M.H., C.M.H., K. Hveem, N.I., A.V.J., I.J., L.A.J., R.S.K., J.R.K., G.K., M. Landén, M. Leboyer, C.M.L., Q.S.L., J. Lissowska, C. Lochner, C. Loughland, N.G.M., C.A.M., F.M., S.L.M., A.M.M., F.J.M., I.M., P. Michie, L. Milani, P. B. Mitchell, G.M., O.M., P. B. Mortensen, B.M., B.M.-M., R.M.M., B.M.N., C.M.N., M.N., M.M.N., M.C.O’D., K.J.O., T.O., M.J.O., S.A.P., C. Pantelis, C. Pato, M.T.P., G.P.P., R.H.P., D.P., J.A.R.-Q., A.R., E.Z.R., M. Ribasés, M. Rietschel, S.R., G.A.R., T.S., U.S., M.S., P.R.S., T.G.S., L.J.S., R.J.S., A.S., C.S.W., J.W.S., H.S., K.S., E. Stordal, F. Streit, P.F.S., G.T., A.E.V., E.V., J.B.V., I.D.W., T.W.W., T.W., N.R.W., J.-A.Z., J.M.B., J.I.N., S. Cichon, H.J.E., E.A.S., A. McQuillin, A.D.F., R.A.O., O.A.A. Bioinformatics: N.M., A.J.F., J.R.I.C., S. Børte, M.J. Gandal, M. Kim, B.M.S., L.G.S., B.S.W., H.-H.W., N.A.-R., S.E.B., B.M.B., V.E.-P., S.H., P.A.H., Y.K., M. Koromina, M. Kubo, M. Leber, P.H.L., C. Liao, L.M.O.L., T.R., P.R., P.D.S., M.S.A., C. Terao, T.E.T., S.X., H.Y., P.P.Z., S. Bengesser, G. Breen, P.F., E.S.G., Q.S.L., G.A.R., H.S., T.W., E.A.S. Clinical: O.K.D., M.I., L. Abramova, K.A., E.A., N.A.-R., A. Anjorin, A. Antoniou, J.H.B., N.B., M. Bauer, A.B., C.B.P., E.B., M.P.B., R.B., M. Brum, N.B.-K., M. Budde, W.B., M. Cairns, M. Casas, P.C., A.C.-B., D.C., P.M.C., N.D., A.D., T. Elvsåshagen, L. Forty, L. Frisén, K.G., J. Garnham, M.G.P., I.R.G., K.G.-S., J. Grove, J.G.-P., K. Ha, M. Haraldsson, M. Hautzinger, U.H., D.H., J. L. Kalman, J. L. Kennedy, S.K.-S., M. Kogevinas, T.M.K., R.K., S.A.K., J. Lawrence, H.-J.L., C. Lewis, S.L., M. Lundberg, D.J.M., W.M., D.M., L. Martinsson, M.M., P. McGuffin, H.M., V.M., C.O’D., L.O., S.P., A. Perry, A. Pfennig, E.P., J.B.P., D.Q., M.H.R., J.R.D., E.J.R., J.P.R., F.R., J.R., E.C.S., F. Senner, E. Sigurdsson, L.S., C.S., O.B.S., D. J. Smith, J.L.S., A.T.S., J.S.S., B.Ś., P.T., M.P.V., H.V., A.H.Y., L.Z., HUNT All-In Psychiatry, R.A., I.A., M.A., G. Babadjanova, L.B., B.T.B., F.B., S. Bengesser, D.H.R.B., A.D.B., A.C., N.C., U.D., D.D., B.E., P.F., M.F., M.G., E.S.G., F.S.G., M. J. Green, M.G.-S., J. Hauser, K.S.H., N.I., I.J., L.A.J., R.S.K., G.K., M. Landén, C.M.L., J. Lissowska, N.G.M., C.A.M., F.M., S.L.M., A.M.M., I.M., P. B. Mitchell, G.M., O.M., P. B. Mortensen, M.C.O’D., K.J.O., M.J.O., C. Pato, M.T.P., R.H.P., J.A.R.-Q., A.R., E.Z.R., M. Rietschel, T.S., T.G.S., A.S., C.S.W., J.W.S., E. Stordal, F. Streit, A.E.V., E.V., J.B.V., I.D.W., T.W.W., T.W., J.I.N., A. McQuillin, A.D.F. Genomic assays/data generation: A.J.F., M.I., E.A., M.A.E., D.A., M.B.-H., E.C.B., C.B.P., J.B.-G., M. Cairns, T.-K.C., C.C., J.C., F.S.D., F.D., S.D., A.F., J.F., N.B.F., J. Gelernter, M.G.P., P.H., S.J., Y.K., H.R.K., M. Kubo, S.E.L., C. Liao, E.M., N.W.M., J.D.M., G.W.M., J.L.M., D.W.M., T.W.M., N.O’B., M. Rivera, C.S.-M., S. Sharp, C.S.H., C. Terao, C. Toma, E.-E.T., S.H.W., HUNT All-In Psychiatry, G. Breen, A.C., T. Esko, J.M.F., E.S.G., D.M.H., N.I., F.J.M., L. Milani, R.M.M., M.M.N., M. Ribasés, G.A.R., T.S., G.T., S. Cichon. Obtained funding for BD samples: M.I., M. Cairns, I.N.F., L. Frisén, S.J., Y.K., J.A.K., M. Kubo, C. Lavebratt, S.L., D.M., P. McGuffin, G.W.M., J.B.P., M.H.R., J.R.D., D. J. Stein, J.S.S., C. Terao, A.H.Y., P.P.Z., M.A., L. Alfredsson, L.B., B.T.B., F.B., W.H.B., M. Boehnke, A.D.B., G. Breen, A.C., N.C., B.E., M.F., J.M.F., E.S.G., M. J. Green, M.G.-S., K.S.H., K. Hveem, N.I., I.J., L.A.J., M. Landén, M. Leboyer, N.G.M., F.J.M., P. B. Mitchell, O.M., P. B. Mortensen, B.M.N., M.N., M.M.N., M.C.O’D., T.O., M.J.O., C. Pato, M.T.P., G.P.P., M. Rietschel, G.A.R., T.S., M.S., P.R.S., T.G.S., C.S.W., J.W.S., G.T., J.B.V., T.W.W., T.W., J.M.B., J.I.N., H.J.E., R.A.O., O.A.A. Statistical analysis: N.M., K.S.O’C., B.C., J.R.I.C., Z.Q., T.D.A., T.B.B., S. Børte, J.B., A.W.C., O.K.D., M. J. Gandal, S.P.H., N.K., M. Kim, K.K., G.P., B.M.S., L.G.S., S. Steinberg, V.T., B.S.W., H.-H.W., V.A., S.A., S.E.B., B.M.B., A.M.D., A.L.D., V.E.-P., T.M.F., O.F., S.D.G., T.A.G., J. Grove, P.A.H., L.H., J.S.J., Y.K., M. Kubo, C. Lavebratt, M. Leber, P.H.L., S.H.M., A. Maihofer, M.M., S.A.M., S.E.M., L.M.O.L., A.F.P., T.R., P.R., D.M.R., O.B.S., C. Terao, T.E.T., J.T.R.W., W.X., J.M.K.Y., H.Y., P.P.Z., H.Z., A.D.B., G. Breen, E.S.G., F.S.G., Q.S.L., B.M.-M., C.M.N., D.P., S.R., H.S., P.F.S., T.W., N.R.W., J.M.B., E.A.S. K.S.O’C., B.C., J.R.I.C. and Z.Q. contributed equally to this work and should be regarded as joint second authors.
Corresponding authors
Correspondence to Niamh Mullins or Ole A. Andreassen .
Ethics declarations
Competing interests.
T.E.T., S. Steinberg, H.S. and K.S. are employed by deCODE Genetics/Amgen. Multiple additional authors work for pharmaceutical or biotechnology companies in a manner directly analogous to academic coauthors and collaborators. A.H.Y. has given paid lectures and served on advisory boards relating to drugs used in affective and related disorders for several companies (AstraZeneca, Eli Lilly, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allergan, Bionomics and Sumitomo Dainippon Pharma), was Lead Investigator for Embolden Study (AstraZeneca), BCI Neuroplasticity study and Aripiprazole Mania Study, and is an investigator for Janssen, Lundbeck, Livanova and Compass. J.I.N. is an investigator for Janssen. P.F.S. reports the following potentially competing financial interests: Lundbeck (advisory committee), Pfizer (Scientific Advisory Board member) and Roche (grant recipient, speaker reimbursement). G. Breen reports consultancy and speaker fees from Eli Lilly and Illumina and grant funding from Eli Lilly. M. Landén has received speaker fees from Lundbeck. O.A.A. has received speaker fees from Lundbeck and Sunovion, and is a consultant to HealthLytix. J.A.R.-Q. was on the speakers bureau and/or acted as consultant for Eli Lilly, Janssen-Cilag, Novartis, Shire, Lundbeck, Almirall, Braingaze, Sincrolab and Rubió in the last 5 years. He also received travel awards (air tickets and hotel) for taking part in psychiatric meetings from Janssen-Cilag, Rubió, Shire and Eli Lilly. The Department of Psychiatry chaired by him received unrestricted educational and research support from the following companies in the last 5 years: Eli Lilly, Lundbeck, Janssen-Cilag, Actelion, Shire, Ferrer, Oryzon, Roche, Psious and Rubió. E.V. has received grants and served as a consultant, advisor or CME speaker for the following entities: AB-Biotics, Abbott, Allergan, Angelini, AstraZeneca, Bristol Myers Squibb, Dainippon Sumitomo Pharma, Farmindustria, Ferrer, Forest Research Institute, Gedeon Richter, GlaxoSmithKline, Janssen, Lundbeck, Otsuka, Pfizer, Roche, SAGE, Sanofi-Aventis, Servier, Shire, Sunovion, Takeda, the Brain and Behaviour Foundation, the Catalan Government (AGAUR and PERIS), the Spanish Ministry of Science, Innovation, and Universities (AES and CIBERSAM), the Seventh European Framework Programme and Horizon 2020 and the Stanley Medical Research Institute. T. Elvsåshagen has received speaker fees from Lundbeck. S.K.-S. received author’s and consultant honoraria from Medice Arzneimittel Pütter GmbH and Shire/Takeda. A.S. is or has been a consultant/speaker for: Abbott, Abbvie, Angelini, AstraZeneca, Clinical Data, Boheringer, Bristol Myers Squibb, Eli Lilly, GlaxoSmithKline, Innovapharma, Italfarmaco, Janssen, Lundbeck, Naurex, Pfizer, Polifarma, Sanofi, Servier. J.R.D. has served as an unpaid consultant to Myriad – Neuroscience (formerly Assurex Health) in 2017 and 2019 and owns stock in CVS Health. H.R.K. serves as an advisory board member for Dicerna Pharmaceuticals, and is a member of the American Society of Clinical Psychopharmacology’s Alcohol Clinical Trials Initiative, which was sponsored in the past 3 years by AbbVie, Alkermes, Amygdala Neurosciences, Arbor Pharmaceuticals, Ethypharm, Indivior, Lilly, Lundbeck, Otsuka and Pfizer. H.R.K. is named as an inventor on PCT patent application no. 15/878,640 entitled: Genotype-guided dosing of opioid agonists, filed January 24, 2018. B.M.N. is a member of the scientific advisory board at Deep Genomics and consultant for Camp4 Therapeutics, Takeda Pharmaceutical and Biogen. All other authors declare no financial interests or potential conflicts of interest.
Additional information
Peer review information Nature Genetics thanks Na Cai, Qiang Wang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information.
Supplementary Figs. 1–9 and Note
Reporting Summary
Peer review information, supplementary tables.
Supplementary Tables 1–23
Supplementary Data 1
Regional association plots
Supplementary Data 2
Forest plots
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mullins, N., Forstner, A.J., O’Connell, K.S. et al. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet 53 , 817–829 (2021). https://doi.org/10.1038/s41588-021-00857-4
Download citation
Received : 02 September 2020
Accepted : 25 March 2021
Published : 17 May 2021
Issue Date : June 2021
DOI : https://doi.org/10.1038/s41588-021-00857-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Breaking down causes, consequences, and mediating effects of telomere length variation on human health.
- Samuel Moix
- Marie C Sadler
- Chiara Auwerx
Genome Biology (2024)
Associations between breakfast skipping and outcomes in neuropsychiatric disorders, cognitive performance, and frailty: a Mendelian randomization study
- Zheng Zhang
- Jinglan Tan
- Qinghua Luo
BMC Psychiatry (2024)
Obstructive sleep apnea and mental disorders: a bidirectional mendelian randomization study
- Xuemei Wang
xWAS analysis in neuropsychiatric disorders by integrating multi-molecular phenotype quantitative trait loci and GWAS summary data
- Lingxue Luo
- Suhua Chang
Journal of Translational Medicine (2024)
Causal links between sedentary behavior, physical activity, and psychiatric disorders: a Mendelian randomization study
Annals of General Psychiatry (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Bipolar Disorder News
Top headlines, latest headlines.
- Reducing the Risk for Bipolar Disorder
- Bipolar Disorder Linked to Early Death
- Light Levels and Mental Health
- Blood Test Can Help Diagnose Bipolar Disorder
- Postpartum Depression Heritability
- Formerly Depressed Still Focus On Negative
- Antidepressants for Bipolar Depression
- Psychiatric Disorders: Shared Genetic ...
- Bipolar Disorder: Scans Capture Brain Changes
- Lithium May Decrease Risk of Developing Dementia
Earlier Headlines
Wednesday, september 25, 2024.
- Digital Biomarkers Shedding Light on Seasonality in Mood Disorders
Tuesday, July 23, 2024
- Bipolar Disorder and Alcohol: It's Not as Simple as 'self-Medication'
Thursday, December 15, 2022
- New Study Reveals Differences in Diagnosis of Psychiatric Disorders Between Geographies
Wednesday, March 9, 2022
- People With Serious Mental Illness May Have Increased Heart Disease Risk at Younger Ages
Thursday, December 23, 2021
- Clues to Treatment of Schizophrenia and Bipolar Disorder Found in Recently Evolved Region of the ‘dark Genome’
Monday, November 29, 2021
- Rates of Type 2 Diabetes Are Higher in People With One of Various Common Psychiatric Disorders
Tuesday, November 2, 2021
- Abnormal Brain Changes Over Time With Bipolar Disorder
- LATEST NEWS
- Top Science
- Top Physical/Tech
- Top Environment
- Top Society/Education
- Health & Medicine
- Mind & Brain
- Disorders and Syndromes
- ADD and ADHD
- Alzheimer's
- Bipolar Disorder
- Borderline Personality Disorder
- Brain Injury
- Hearing Impairment
- Huntington's Disease
- Mad Cow Disease
- Multiple Sclerosis
- Obstructive Sleep Apnea
- Parkinson's
- Schizophrenia
- Sleep Disorders
- Education & Learning
- Brain-Computer Interfaces
- Educational Psychology
- Infant and Preschool Learning
- Intelligence
- K-12 Education
- Language Acquisition
- Learning Disorders
- Illegal Drugs
- Crystal Meth
- Psychedelic Drugs
- Living Well
- Anger Management
- Child Development
- Consumer Behavior
- Dieting and Weight Control
- Gender Difference
- Nutrition Research
- Racial Issues
- Relationships
- Spirituality
- Mental Health
- Eating Disorders
- Smoking Addiction
- Neuroscience
- Child Psychology
- Social Psychology
- Space & Time
- Matter & Energy
- Computers & Math
- Plants & Animals
- Earth & Climate
- Fossils & Ruins
- Science & Society
- Business & Industry
Strange & Offbeat
- Gut Bacteria Transfer Genes to Beat ...
- Fire-Risk Blocking Hydrogen Production System
- Tiny Electric Currents May Cut Skin Infections
- Grain-Sized Soft Robots for Drug Delivery
- PFAS: US Drinking Water Contamination
- Chronic Pain Predicted Within 3 Days of Injury
- Electric Cars: Long-Lasting Renewable Batteries
- Wildfires Becoming Faster, More Dangerous
- Beyond Superheavy Element Livermorium
- Weight-Loss Drug May Cut Alzheimer's Risk
Trending Topics
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Diagnosis and...
Diagnosis and management of bipolar disorders
- Related content
- Peer review
- 1 Precision Medicine Center of Excellence in Mood Disorders, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
- 2 Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA
- Correspondence to: F S Goes fgoes1{at}jhmi.edu
Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world’s population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a leading cause of disability and premature mortality. The clinical manifestations of bipolar disorder can be markedly varied between and within individuals across their lifespan. Early diagnosis is challenging and misdiagnoses are frequent, potentially resulting in missed early intervention and increasing the risk of iatrogenic harm. Over 15 approved treatments exist for the various phases of bipolar disorder, but outcomes are often suboptimal owing to insufficient efficacy, side effects, or lack of availability. Lithium, the first approved treatment for bipolar disorder, continues to be the most effective drug overall, although full remission is only seen in a subset of patients. Newer atypical antipsychotics are increasingly being found to be effective in the treatment of bipolar depression; however, their long term tolerability and safety are uncertain. For many with bipolar disorder, combination therapy and adjunctive psychotherapy might be necessary to treat symptoms across different phases of illness. Several classes of medications exist for treating bipolar disorder but predicting which medication is likely to be most effective or tolerable is not yet possible. As pathophysiological insights into the causes of bipolar disorders are revealed, a new era of targeted treatments aimed at causal mechanisms, be they pharmacological or psychosocial, will hopefully be developed. For the time being, however, clinical judgment, shared decision making, and empirical follow-up remain essential elements of clinical care. This review provides an overview of the clinical features, diagnostic subtypes, and major treatment modalities available to treat people with bipolar disorder, highlighting recent advances and ongoing therapeutic challenges.
Introduction
Abnormal states of mood, ranging from excesses of despondency, psychic slowness, diminished motivation, and impaired cognitive functioning on the one hand, and exhilaration, heightened energy, and increased cognitive and motoric activity on the other, have been described since antiquity. 1 However, the syndrome in which both these pathological states occur in a single individual was first described in the medical literature in 1854, 2 although its fullest description was made by the German psychiatrist Emil Kraepelin at the turn of the 19th century. 3 Kraepelin emphasized the periodicity of the illness and proposed an underlying trivariate model of mood, thought (cognition), and volition (activity) to account for the classic forms of mania and depression and the various admixed presentations subsequently know as mixed states. 3 These initial descriptions of manic depressive illness encompassed most recurrent mood syndromes with relapsing remitting course, minimal interepisode morbidity, and a wide spectrum of “colorings of mood” that pass “without a sharp boundary” from the “rudiment of more severe disorders…into the domain of personal predisposition.” 3 Although Kraepelin’s clinical description of bipolar disorder (BD) remains the cornerstone of today’s clinical description, more modern conceptions of bipolar disorder have differentiated manic depressive illness from recurrent depression, 4 partly based on differences in family history and the relative specificity of lithium carbonate and mood stabilizing anticonvulsants as anti-manic and prophylactic agents in bipolar disorder. While the boundaries of bipolar disorder remain a matter of controversy, 5 this review will focus on modern clinical conceptions of bipolar disorder, highlighting what is known about its causes, prognosis, and treatments, while also exploring novel areas of inquiry.
Sources and selection criteria
PubMed and Embase were searched for articles published from January 2000 to February 2023 using the search terms “bipolar disorder”, “bipolar type I”, “bipolar type II”, and “bipolar spectrum”, each with an additional search term related to each major section of the review article (“definition”, “diagnosis”, “nosology”, “prevalence”, “epidemiology”, “comorbid”, “precursor”, “prodrome”, “treatment”, “screening”, “disparity/ies”, “outcome”, “course”, “genetics”, “imaging”, “treatment”, “pharmacotherapy”, “psychotherapy”, “neurostimulation”, “convulsive therapy”, “transmagnetic”, “direct current stimulation”, “suicide/suicidal”, and “precision”). Searches were prioritized for systematic reviews and meta-analyses, followed by randomized controlled trials. For topics where randomized trials were not relevant, searches also included narrative reviews and key observational studies. Case reports and small observations studies or randomized controlled trials of fewer than 50 patients were excluded.
Modern definitions of bipolar disorder
In the 1970s, the International Classification of Diseases and the Diagnostic and Statistical Manual of Mental Disorders reflected the prototypes of mania initially described by Kraepelin, following the “neo-Kraepelinian” model in psychiatric nosology. To meet the primary requirement for a manic episode, an individual must experience elevated or excessively irritable mood for at least a week, accompanied by at least three other typical syndromic features of mania, such as increased activity, increased speed of thoughts, rapid speech, changes in esteem, decreased need for sleep, or excessive engagement in impulsive or pleasurable activities. Psychotic symptoms and admission to hospital can be part of the diagnostic picture but are not essential to the diagnosis. In 1994, Diagnostic and Statistical Manual of Mental Disorders , fourth edition (DSM-IV) carved out bipolar disorder type II (BD-II) as a separate diagnosis comprising milder presentations of mania called hypomania. The diagnostic criteria for BD-II are similar to those for bipolar disorder type I (BD-I), except for a shorter minimal duration of symptoms (four days) and the lack of need for significant role impairment during hypomania, which might be associated with enhanced functioning in some individuals. While the duration criteria for hypomania remain controversial, BD-II has been widely accepted and shown to be as common as (if not more common than) BD-I. 6 The ICD-11 (international classification of diseases, 11th revision) included BD-II as a diagnostic category in 2019, allowing greater flexibility in its requirement of hypomania needing to last several days.
The other significant difference between the two major diagnostic systems has been their consideration of mixed symptoms. Mixed states, initially described by Kraepelin as many potential concurrent combinations of manic and depressive symptoms, were more strictly defined by DSM as a week or more with full syndromic criteria for both manic and depressive episodes. In DSM-5, this highly restrictive criterion was changed to encompass a broader conception of subsyndromal mixed symptoms (consisting of at least three contrapolar symptoms) in either manic, hypomanic, or depressive episodes. In ICD-11, mixed symptoms are still considered to be an episode, with the requirement of several prominent symptoms of the countervailing mood state, a less stringent requirement that more closely aligns with Kraepelin's broader conception of mixed states. 7
Epidemiology
Using DSM-IV criteria, the National Comorbidity Study replication 6 found similar lifetime prevalence rates for BD-I (1.0%) and BD-II (1.1%) among men and women. Subthreshold symptoms of hypomania (bipolar spectrum disorder) were more common, with prevalence rate estimates of 2.4%. 6 Incidence rates, which largely focus on BD-I, have been estimated at approximately 6.1 per 100 000 person years (95% confidence interval 4.7 to 8.1). 8 Estimates of the incidence and lifetime prevalence of bipolar disorder show moderate variations according to the method of diagnosis (performed by lay interviewers in a research context v clinically trained interviews) and the racial, ethnic, and demographic context. 9 Higher income, westernized countries have slightly higher rates of bipolar disorder, 10 which might reflect a combination of westernized centricity in the specific idioms used to understand and elicit symptoms, as well as a greater knowledge, acceptance, and conceptualization of emotional symptoms as psychiatric disorders.
Causes of bipolar disorder
Like other common psychiatric disorders, bipolar disorder is likely caused by a complex interplay of multiple factors, both at the population level and within individuals, 11 which can be best conceptualized at various levels of analysis, including genetics, brain networks, psychological functioning, social support, and other biological and environmental factors. Because knowledge about the causes of bipolar disorder remains in its infancy, for pragmatic purposes, most research has followed a reductionistic model that will ultimately need to be synthesized for a more coherent view of the pathophysiology that underlies the condition.
Insights from genetics
From its earliest descriptions, bipolar disorder has been observed to run in families. Indeed, family history is the strongest individual risk factor for developing the disorder, with first degree relatives having an approximately eightfold higher risk of developing bipolar disorder compared with the baseline population rates of ~1%. 12 While family studies cannot separate the effects of genetics from behavioral or cultural transmission, twin and adoption studies have been used to confirm that the majority of the familial risk is genetic in origin, with heritability estimates of approximately 60-80%. 13 14 There have been fewer studies of BD-II, but its heritability has been found to be smaller (~46%) 15 and closer to that of more common disorders such as major depressive disorder or generalized anxiety. 15 16 Nevertheless, significant heritability does not necessarily imply the presence of genes of large effect, since the genetic risk for bipolar disorder appears likely to be spread across many common variants of small effect sizes. 16 17 Ongoing studies of rare variations have found preliminary evidence for variants of slightly higher effect sizes, with initial evidence of convergence with common variations in genes associated with the synapse and the postsynaptic density. 18 19
While the likelihood that the testing of single variants or genes will be useful for diagnostic purposes is low, analyses known as polygenic risk studies can sum across all the risk loci and have some ability to discriminate cases from controls, albeit at the group level rather than the individual level. 20 These polygenic risk scores can also be used to identify shared genetic risk factors across other medical and psychiatric disorders. Bipolar disorder has strong evidence for common variant based coheritability with schizophrenia (genetic correlation (r g ) 0.69) and major depressive disorder (r g 0.48). BD-I has stronger coheritability with schizophrenia compared with BD-II, which is more strongly genetically correlated with major depressive disorder (r g 0.66). 16 Lower coheritability was observed with attention deficit hyperactivity disorder (r g 0.21), anorexia nervosa (0.20), and autism spectrum disorder (r g 0.21). 16 These correlations provide evidence for shared genetic risk factors between bipolar disorder and other major psychiatric syndromes, a pattern also corroborated by recent nationwide registry based family studies. 12 14 Nevertheless, despite their potential usefulness, polygenic risk scores must currently be interpreted with caution given their lack of populational representation and lingering concerns of residual confounds such as gene-environment correlations. 21
Insights from neuroimaging
Similarly to the early genetic studies, small initial studies had limited replication, leading to the formation of large worldwide consortiums such as ENIGMA (enhancing neuroimaging genetics through meta-analysis) which led to substantially larger sample sizes and improved reproducibility. In its volumetric analyses of subcortical structures from MRI (magnetic resonance imaging) of patients with bipolar disorder, the ENIGMA consortium found modest decreases in the volume of the thalamus (Cohen’s d −0.15), the hippocampus (−0.23), and the amygdala (−0.11), with an increased volume seen only in the lateral ventricles (+0.26). 22 Meta-analyses of cortical regions similarly found small reductions in cortical thickness broadly across the parietal, temporal, and frontal cortices (Cohen’s d −0.11 to −0.29) but no changes in cortical surface area. 23 In more recent meta-analyses of white matter tracts using diffuse tension imaging, widespread but modest decreases in white matter integrity were found throughout the brain in bipolar disorder, most notably in the corpus callosum and bilateral cinguli (Cohen’s d −0.39 to −0.46). 24 While these findings are likely to be highly replicable, they do not, as yet, have clinical application. This is because they reflect differences at a group level rather than an individual level, 25 and because many of these patterns are also seen across other psychiatric disorders 26 and could be either shared risk factors or the effects of confounding factors such as medical comorbidities, medications, co-occurring substance misuse, or the consequences (rather than causes) of living with mental illness. 27 Efforts to collate and meta-analyze large samples utilizing longitudinal designs 28 task based, resting state functional MRI measurents, 29 as well as other measures of molecular imaging (magnetic resonance spectroscopy and positron emission tomography) are ongoing but not as yet synthesized in large scale meta-analyses.
Environmental risk factors
Because of the difficulty in measuring and studying the relevant and often common environmental risk factors for a complex illness like bipolar disorder, there has been less research on how environmental risk factors could cause or modify bipolar disorder. Evidence for intrauterine risk factors is mixed and less compelling than such evidence in disorders like schizophrenia. 30 Preliminary evidence suggests that prominent seasonal changes in solar radiation, potentially through its effects on circadian rhythm, can be associated with an earlier onset of bipolar disorder 31 and a higher likelihood of experiencing a depressive episode at onset. 31 However, the major focus of environmental studies in bipolar disorder has been on traumatic and stressful life events in early childhood 32 and in adulthood. 33 The effects of such adverse events are complex, but on a broad level have been associated with earlier onset of bipolar disorder, a worse illness course, greater prevalence of psychotic symptoms, 34 substance misuse and psychiatric comorbidities, and a higher risk of suicide attempts. 32 35 Perhaps uniquely in bipolar disorder, evidence also indicates that positive life events associated with goal attainment can also increase the risk of developing elevated states. 36
Comorbidity
Bipolar disorder rarely manifests in isolation, with comorbidity rates indicating elevated lifetime risk of several co-occurring symptoms and comorbid disorders, particularly anxiety, attentional disorders, substance misuse disorders, and personality disorders. 37 38 The causes of such comorbidity can be varied and complex: they could reflect a mixed presentation artifactually separated by current diagnostic criteria; they might also reflect independent illnesses; or they might represent the downstream effects of one disorder increasing the risk of developing another disorder. 39 Anxiety disorders tend to occur before the frank onset of manic or hypomanic symptoms, suggesting that they could in part reflect prodromal symptoms that manifest early in the lifespan. 37 Similarly, subthreshold and syndromic symptoms of attention deficit/hyperactivity disorder are also observed across the lifespan of people with bipolar disorder, but particularly in early onset bipolar disorder. 40 On the other hand, alcohol and substance misuse disorders occur more evenly before and after the onset of bipolar disorder, consistent with a more bidirectional causal association. 41
The association between bipolar disorder and comorbid personality disorders is similarly complex. Milder manifestations of persistent mood instability (cyclothymia) or low mood (dysthymia) have previously been considered to be temperamental variants of bipolar disorder, 42 but are now classified as related but separate disorders. In people with persistent emotional dysregulation, making the diagnosis of bipolar disorder can be particularly challenging, 43 since the boundaries between longstanding mood instability and phasic changes in mood state can be difficult to distinguish. While symptom overlap can lead to artificially inflated prevalence rates of personality disorders in bipolar disorder, 44 the elevated rates of most personality disorders in bipolar disorder, particularly those related to emotional instability, are likely reflective of an important clinical phenomenon that is understudied, particularly with regard to treatment implications. 45 In general, people with comorbidities tend to have greater symptom burden and functional impairment and have lower response rates to treatment. 46 47 Data on approaches to treat specific comorbid disorders in bipolar disorder are limited, 48 49 and clinicians are often left to rely on their clinical judgment. The most parsimonious approach is to treat primary illness as fully as possible before considering additional treatment options for remaining comorbid symptoms. For certain comorbidities, such as anxiety symptoms and disorders of attention, first line pharmacological treatment—namely, antidepressants and stimulants, should be used with caution, since they might increase the long term risks of mood switching or overall mood instability. 50 51
Like other major mental illnesses, bipolar disorder is also associated with an increased prevalence of common medical disorders such as obesity, hyperlipidemia, coronary artery disease, chronic obstructive pulmonary disease, and thyroid dysfunction. 52 These have been attributed to increase risk factors such as physical inactivity, poor nutrition, smoking, and increased use of addictive substances, 53 but some could also be consequences of specific treatments, such as the atypical antipsychotics and mood stabilizers. 54 Along with poor access to care, this medical burden likely accounts for much of the increased standardized mortality (approximately 2.6 times higher) in people with bipolar disorder, 55 highlighting the need to utilize treatments with better long term side effect profiles, and the need for better integration with medical care.
Precursors and prodromes: who develops bipolar disorder?
While more widespread screening and better accessibility to mental health providers should in principle shorten the time to diagnosis and treatment, early manifestation of symptoms in those who ultimately go on to be diagnosed with bipolar disorder is generally non-specific. 56 In particular, high risk offspring studies of adolescents with a parent with bipolar disorder have found symptoms of anxiety and attentional/disruptive disorders to be frequent in early adolescence, followed by higher rates of depression and sleep disturbance in later teenage years. 56 57 Subthreshold symptoms of mania, such as prolonged increases in energy, elated mood, racing thoughts, and mood lability are also more commonly found in children with prodromal symptoms (meta-analytic prevalence estimates ranging from 30-50%). 58 59 Still, when considered individually, none of these symptoms or disorders are sensitive or specific enough to accurately identify individuals who will transition to bipolar disorder. Ongoing approaches to consider these clinical factors together to improve accuracy have a promising but modest ability to identify people who will develop bipolar disorder, 60 emphasizing the need for further studies before implementation.
Screening for bipolar disorder
Manic episodes can vary from easily identifiable prototypical presentations to milder or less typical symptoms that can be challenging to diagnose. Ideally, a full diagnostic evaluation with access to close informants is performed on patients presenting to clinical care; however, evaluations can be hurried in routine clinical care, and the ability to recall previous episodes might be limited. In this context, the use of screening scales can be a helpful addition to clinical care, although screening scales must be regarded as an impetus for a confirmatory clinical interview rather than a diagnostic instrument by themselves. The two most widely used and openly available screening scales are the mood disorders questionnaire (based on the DSM-IV criteria for hypomania) 61 and the hypomania check list (HCL-32), 62 that represent a broader overview of symptoms proposed to be part of a broader bipolar spectrum.
Racial/ethnic disparities
Although community surveys using structured or semi-structured diagnostic instruments, have provided little evidence for variation across ethnic groups, 63 64 observational studies based on clinical diagnoses in healthcare settings have found a disproportionately higher rate of diagnosis of schizophrenia relative to bipolar disorder in black people. 65 Consistent with similar disparities seen across medicine, these differences in clinical diagnoses are likely influenced by a complex mix of varying clinical presentations, differing rates of comorbid conditions, poorer access to care, greater social and economic burden, as well as the potential effect of subtle biases of healthcare professionals. 65 While further research is necessary to identify driving factors responsible for diagnostic disparities, clinicians should be wary of making a rudimentary diagnosis in patients from marginalized backgrounds, ensuring comprehensive data gathering and a careful diagnostic formulation that incorporates shared decision making between patient and provider.
Bipolar disorder is a recurrent illness, but its longitudinal course is heterogeneous and difficult to predict. 46 66 The few available long term studies of BD-I and BD-II have found a consistent average rate of recurrence of 0.40 mood episodes per year in historical studies 67 and 0.44 mood episodes per year in more recent studies. 68 The median time to relapse is estimated to be 1.44 years, with higher relapse rates seen in BD-I (0.81 years) than in BD-II (1.63 years) and no differences observed with respect to age or sex. 1 2 In addition to focusing on episodes, an important development in research and clinical care of bipolar disorder has been the recognition of the burden of subsyndromal symptoms. Although milder in severity, these symptoms can be long lasting, functionally impairing, and can themselves be a risk factor for episode relapse. 69 Recent cohort studies have also found that a substantial proportion of patients with bipolar disorder (20-30%) continue to have poor outcomes even after receiving guideline based care. 46 70 Risk factors that contribute to this poor outcome include transdiagnostic indicators of adversity such as substance misuse, low educational attainment, socioeconomic hardship, and comorbid disorders. As expected, those with more severe past illness activity, including those with rapid cycling, were also more likely to remain symptomatically and psychosocially impaired. 46 71 72
The primary focus of treating bipolar disorder has been to manage the manic, mixed, or depressive episodes that present to clinical care and to subsequently prevent recurrence of future episodes. Owing to the relapse remitting nature of the illness, randomized controlled trials are essential to determine treatment efficacy, as the observation of clinical improvement could just represent the ebbs and flows of the natural history of the illness. In the United States, the FDA (Food and Drug Administration) requires at least two large scale placebo controlled trials (phase 3) to show significant evidence of efficacy before approving a treatment. Phase 3 studies of bipolar disorder are generally separated into short term studies of mania (3-4 weeks), short term studies for bipolar depression (4-6 weeks), and longer term maintenance studies to evaluate prophylactic activity against future mood episodes (usually lasting one year). Although the most rigorous evaluation of phase 3 studies would be to require two broadly representative and independent randomized controlled trials, the FDA permits consideration of so called enriched design trials that follow participants after an initial response and tolerability has been shown to an investigational drug. Because of this initial selection, such trials can be biased against comparator agents, and could be less generalizable to patients seen in clinical practice.
A summary of the agents approved by the FDA for treatment of bipolar disorder is in table 1 , which references the key clinical trials demonstrating efficacy. Figure 1 and supplementary table 1 are a comparison of treatments for mania, depression, and maintenance. Effect sizes reflect the odds ratios or relative risks of obtaining response (defined as ≥50% improvement from baseline) in cases versus controls and were extracted from meta-analyses of randomized controlled trials for bipolar depression 86 and maintenance, 94 as well as a network meta-analysis of randomized controlled trials in bipolar mania. 73 Effect sizes are likely to be comparable for each phase of treatment, but not across the different phases, since methodological differences exist between the three meta-analytic studies.
FDA approved medications for bipolar disorder
- View inline

Summary of treatment response rates (defined as ≥50% improvement from baseline) of modern clinical trials for acute mania, acute bipolar depression, and long term recurrence. Meta-analytic estimates were extracted from recent meta-analyses or network meta-analyses of acute mania, 73 acute bipolar depression, 86 and bipolar maintenance studies 94
- Download figure
- Open in new tab
- Download powerpoint
Acute treatment of mania
As mania is characterized by impaired judgment, individuals can be at risk for engaging in high risk, potentially dangerous behaviors that can have substantial personal, occupational, and financial consequences. Therefore, treatment of mania is often considered a psychiatric emergency and is, when possible, best performed in the safety of an inpatient unit. While the primary treatment for mania is pharmacological, diminished insight can impede patients' willingness to accept treatment, emphasizing the significance of a balanced therapeutic approach that incorporates shared decision making frameworks as much as possible to promote treatment adherence.
The three main classes of anti-manic treatments are lithium, mood stabilizing anticonvulsants (divalproate and carbamazepine), and antipsychotic medications. Almost all antipsychotics are effective in treating mania, with the more potent dopamine D2 receptor antagonists such as risperidone and haloperidol demonstrating slightly higher efficacy ( fig 1 ). 73 In the United States, the FDA has approved the use of all second generation antipsychotics for treating mania except for lurasidone and brexpriprazole. Compared with mood stabilizing medications, second generation antipsychotics have a faster onset of action, making them a first line treatment for more severe manic symptoms that require rapid treatment. 99 The choice of which specific second generation antipsychotic to use depends on a balance of efficacy, tolerability concerns, and cost considerations (see table 1 ). Notably, the FDA has placed a black box warning on all antipsychotics for increasing the risk of cerebral vascular accidents in the elderly. 100 While this was primarily focused on the use of antipsychotics in dementia, this likely class effect should be taken into account when considering the use of antipsychotics in the elderly.
Traditional mood stabilizers, such as lithium, divalproate, and carbamazepine are also effective in the treatment of active mania ( fig 1 ). Since lithium also has a robust prophylactic effect (see section on prevention of mood episodes below) it is often recommended as first line treatment and can be considered as monotherapy when rapid symptom reduction is not clinically indicated. On the other hand, other anticonvulsants such as lamotrigine, gabapentin, topiramate, and oxcarbazepine have not been found to be effective for the treatment of mania or mixed episodes. 101 Although the empirical evidence for polypharmacy is limited, 102 combination treatment in acute mania, usually consisting of a mood stabilizer and a second generation antipsychotic, is commonly used in clinical practice despite the higher burden of side effects. Following resolution of an acute mania, consideration should be given to transitioning to monotherapy with an agent with proven prophylactic activity.
Pharmacological approaches to bipolar depression
Depressed episodes are usually more common than mania or hypomania, 103 104 and often represent the primary reason for individuals with bipolar disorder to seek treatment. Nevertheless, because early antidepressant randomized controlled trials did not distinguish between unipolar and bipolar depressive episodes, it has only been in the past two decades that large scale randomized controlled trials have been conducted specifically for bipolar depression. As such trials are almost exclusively funded by pharmaceutical companies, they have focused on the second generation antipsychotics and newer anticonvulsants still under patent. These trials have shown moderate but robust effects for most recent second generation antipsychotics, five of which have received FDA approval for treating bipolar depression ( table 1 ). No head-to-head trials have been conducted among these agents, so the choice of medication depends on expected side effects and cost considerations. For example, quetiapine has robust antidepressant efficacy data but is associated with sedation, weight gain, and adverse cardiovascular outcomes. 105 Other recently approved medications such as lurasidone, cariprazine, and lumateperone have better side effect profiles but show more modest antidepressant activity. 106
Among the mood stabilizing anticonvulsants, lamotrigine has limited evidence for acute antidepressant activity, 107 possibly owing to the need for an 8 week titration to reach the full dose of 200 mg. However, as discussed below, lamotrigine can still be considered for mild to moderate acute symptoms owing to its generally tolerable side effect profile and proven effectiveness in preventing the recurrence of depressive episodes. Divalproate and carbamazepine have some evidence of being effective antidepressants in small studies, but as there has been no large scale confirmatory study, they should be considered second or third line options. 86 Lithium has been studied for the treatment of bipolar depression as a comparator to quetiapine and was not found to have a significant acute antidepressant effect. 88
Antidepressants
Owing to the limited options of FDA approved medications for bipolar depression and concerns of metabolic side effects from long term second generation antipsychotic use, clinicians often resort to the use of traditional antidepressants for the treatment of bipolar depression 108 despite the lack of FDA approval for such agents. Indeed, recent randomized clinical trials of antidepressants in bipolar depression have not shown an effect for paroxetine, 89 109 bupropion, 109 or agomelatine. 110 Beyond the question of efficacy, another concern regarding antidepressants in bipolar disorder is their potential to worsen the course of illness by either promoting mixed or manic symptoms or inducing more subtle degrees of mood instability and cycle acceleration. 111 However, the risk of switching to full mania while being treated with mood stabilizers appears to be modest, with a meta-analysis of randomized clinical trials and clinical cohort studies showing the rates of mood switching over an average follow-up of five months to be approximately 15.3% in people with bipolar disorder treated on antidepressants compared with 13.8% in those without antidepressant treatment. 111 The risk of switching appears to be higher in the first 1-2 years of treatment in people with BD-I, and in those treated with a tricyclic antidepressant 112 or the dual reuptake inhibitor venlafaxine. 113 Overall, while the available data have methodological limitations, most guidelines do not recommend the use of antidepressants in bipolar disorder, or recommend them only after agents with more robust evidence have been tried. That they remain so widely used despite the equivocal evidence base reflects the unmet need for treatment of depression, concerns about the long term side effects of second generation antipsychotics, and the challenges of changing longstanding prescribing patterns.
Pharmacological approaches to prevention of recurrent episodes
Following treatment of the acute depressive or manic syndrome, the major focus of treatment is to prevent future episodes and minimize interepisodic subsyndromal symptoms. Most often, the medication that has been helpful in controlling the acute episode can be continued for prevention, particularly if clinical trial evidence exists for a maintenance effect. To show efficacy for prevention, studies must be sufficiently long to allow the accumulation of future episodes to occur and be potentially prevented by a therapeutic intervention. However, few long term treatment studies exist and most have utilized enriched designs that likely favor the drug seeking regulatory approval. As shown in figure 1 , meta-analyses 94 show prophylactic effect for most (olanzapine, risperidone, quetiapine, aripiprazole, asenapine) but not all (lurasidone, paliperidone) recently approved second generation antipsychotics. The effect sizes are generally comparable with monotherapy (odds ratio 0.42, 95% confidence interval 0.34 to 0.5) or as adjunctive therapy (odds ratio 0.37, 95% confidence interval 0.25 to 0.55). 94 Recent studies of lithium, which have generally used it as a (non-enriched) comparator drug, show a comparable protective effect (odds ratio 0.46, 95% confidence interval 0.28 to 0.75). 94 Among the mood stabilizing anticonvulsant drugs, a prophylactic effect has also been found for both divalproate and lamotrigine ( fig 1 and supplementary table 1), although only the latter has been granted regulatory approval for maintenance treatment. While there are subtle differences in effect sizes in drugs approved for maintenance ( fig 1 and table 1 ), the overlapping confidence intervals and methodological differences between studies prevent a strict comparison of the effect measures.
Guidelines often recommend lithium as a first line agent given its consistent evidence of prophylaxis, even when tested as the disadvantaged comparator drug in enriched drug designs. Like other medications, lithium has a unique set of side effects and ultimately the decision about which drug to use among those which are efficacious should be a decision carefully weighed and shared between patient and provider. The decision might be re-evaluated after substantial experience with the medication or at different stages in the long term treatment of bipolar disorder (see table 1 ).
Psychotherapeutic approaches
The frequent presence of residual symptoms, often associated with psychosocial and occupational dysfunction, has led to renewed interest in psychotherapeutic and psychosocial approaches to bipolar disorder. Given the impairment of judgment seen in mania, psychotherapy has more of a supportive and educational role in the treatment of mania, whereas it can be more of a primary focus in the treatment of depressive states. On a broad level, psychotherapeutic approaches effective for acute depression, such as cognitive behavioral therapy, interpersonal therapy, behavioral activation, and mindfulness based strategies, can also be recommended for acute depressive states in individuals with bipolar disorder. 114 Evidence for more targeted psychotherapy trials for bipolar disorder is more limited, but meta-analyses have found evidence for decreased recurrence (odds ratio 0.56; 95% confidence interval 0.43 to 0.74) 115 and improvement of subthreshold interepisodic depressive and manic symptoms with cognitive behavioral therapy, family based therapy, interpersonal and social rhythm therapy, and psychoeducation. 115 Recent investigations have also focused on targeted forms of psychotherapy to improve cognition 116 117 118 as well as psychosocial and occupational functioning. 119 120 Although these studies show evidence of a moderate effect, they remain preliminary, methodologically diverse, and require replication on a larger scale. 121
The implementation of evidence based psychotherapy as a treatment faces several challenges, including clinical training, fidelity monitoring, and adequate reimbursement. Novel approaches, leveraging the greater tractability of digital tools 122 and allied healthcare workers, 123 are promising means of lessening the implementation gap; however, these approaches require validation and evidence of clinical utility similar to traditional methods.
Neurostimulation approaches
For individuals with bipolar disorder who cannot tolerate or do not respond well to standard pharmacotherapy or psychotherapeutic approaches, neurostimulation techniques such as repetitive transcranial magnetic stimulation or electric convulsive therapy should be considered as second or third line treatments. Electric convulsive therapy has shown response rates of approximately 60-80% in severe acute depressions 124 125 and 50-60% in cases with treatment resistant depression. 126 These response rates compare favorably with those of pharmacological treatment, which are likely to be closer to ~50% and ~30% in subjects with moderate to severe depression and treatment resistant depression, respectively. 127 Although the safety of electric convulsive therapy is well established, relatively few medical centers have it available, and its acceptability is limited by cognitive side effects, which are usually short term, but which can be more significant with longer courses and with bilateral electrode placement. 128 While there have been fewer studies of electric convulsive therapy for bipolar depression compared with major depressive disorder, it appears to be similarly effective and might show earlier response. 129 Anecdotal evidence also suggests electric convulsive therapy that is useful in refractory mania. 130
Compared with electric convulsive therapy, repetitive transcranial magnetic stimulation has no cognitive side effects and is generally well tolerated. Repetitive transcranial magnetic stimulation acts by generating a magnetic field to depolarize local neural tissue and induce excitatory or inhibitory effects depending on the frequency of stimulation. The most studied FDA approved form of repetitive transcranial magnetic stimulation applies high frequency (10 Hz) excitatory pulses to the left prefrontal cortex for 30-40 minutes a day for six weeks. 131 Like electric convulsive therapy, repetitive transcranial magnetic stimulation has been primarily studied in treatment resistant depression and has been found to have moderate effect, with about one third of patients having a significant treatment response compared with those treated with pharmacotherapy. 131 Recent innovations in transcranial magnetic stimulation have included the use of a novel, larger coil to stimulate a larger degree of the prefrontal cortex (deep transcranial magnetic stimulation), 132 and a shortened (three minutes), higher frequency intermittent means of stimulation known as theta burst stimulation that appears to be comparable to conventional (10 Hz) repetitive transcranial magnetic stimulation. 133 A preliminary trial has recently assessed a new accelerated protocol of theta burst stimulation marked by 10 sessions a day for five days. It found that theta burst stimulation had a greater effect on people with treatment resistant depression compared with treatment as usual, although larger studies are needed to confirm these findings. 134
Conventional repetitive transcranial magnetic stimulation (10 Hz) studies in bipolar disorder have been limited by small sample sizes but have generally shown similar effects compared with major depressive disorder. 135 However, a proof of concept study of single session theta burst stimulation did not show efficacy in bipolar depression, 136 reiterating the need for specific trials for bipolar depression. Given the lack of such trials in bipolar disorder, repetitive transcranial magnetic stimulation should be considered a potentially promising but as yet unproven treatment for bipolar depression.
The other major form of neurostimulation studied in both unipolar and bipolar depression is transcranial direct current stimulation, an easily implemented method of delivering a low amplitude electrical current to the prefrontal area of the brain that could lead to local changes in neuronal excitability. 137 Like repetitive transcranial magnetic stimulation, transcranial direct current stimulation is well tolerated and has been mostly studied in unipolar depression, but has not yet generated sufficient evidence to be approved by a regulatory agency. 138 Small studies have been performed in bipolar depression, but the results have been mixed and require further research before use in clinical settings. 137 138 139 Finally, the evidence for more invasive neurostimulation studies such as vagal nerve stimulation and deep brain stimulation remains extremely limited and is currently insufficient for clinical use. 140 141
Treatment resistance in bipolar disorder
As in major depressive disorder, the use of term treatment resistance in bipolar disorder is controversial since differentiating whether persistent symptoms are caused by low treatment adherence, poor tolerability, the presence of comorbid disorders, or are the result of true treatment resistance, is an essential but often challenging clinical task. Treatment resistance should only be considered after two or three trials of evidence based monotherapy, adjunctive therapy, or both. 142 In difficult-to-treat mania, two or more medications from different mechanistic classes are typically used, with electric convulsive therapy 143 and clozapine 144 being considered if more conventional anti-manic treatments fail. In bipolar depression, it is common to combine antidepressants with anti-manic agents, despite limited evidence for efficacy. 145 Adjunctive therapies such as bright light therapy, 146 the dopamine D2/3 receptor agonist pramipexole, 147 and ketamine 148 149 have shown promising results in small open label trials that require further study.
Treatment considerations to reduce suicide in bipolar disorder
The risk of completed suicide is high across the subtypes of bipolar disorder, with estimated rates of 10-15% across the lifespan. 150 151 152 Lifetime rates of suicide attempts are much higher, with almost half of all individuals with bipolar disorder reporting at least one attempt. 153 Across a population and, often within individuals, the causes of suicide attempts and completed suicides are likely to be multifactorial, 154 affected by various risk factors, such as symptomatic illness, environmental stressors, comorbidities (particularly substance misuse), trait impulsivity, interpersonal conflict, loneliness, or socioeconomic distress. 155 156 Risk is highest in depressive and dysphoric/mixed episodes 157 158 and is particularly high in the transitional period following an acute admission to hospital. 159 Among the available treatments, lithium has potential antisuicidal properties. 160 However, since suicide is a rare event, with very few to zero suicides within a typical clinical trial, moderate evidence for this effect emerges only in the setting of meta-analyses of clinical trials. 160 Several observational studies have shown lower mortality in patients on lithium treatment, 161 but such associations might not be causal, since lithium is potentially fatal in overdose and is often avoided by clinicians in patients at high risk of suicide.
The challenge of studying scarce events has led most studies to focus on the reduction of the more common phenomena of suicidal ideation and behavior as a proxy for actual suicides. A recent such multisite study of the Veterans Affairs medical system included a mixture of unipolar and bipolar disorder and was stopped prematurely for futility, indicating no overall effect of moderate dose lithium. 162 Appropriate limitations of this study have been noted, 163 164 including difficulties in recruitment, few patients with bipolar disorder (rather than major depressive disorder), low levels of compliance with lithium therapy, high rates of comorbidity, and a follow-up of only one year. Nevertheless, while the body of evidence suggests that lithium has a modest antisuicidal effect, its degree of protection and utility in complex patients with comorbidities and multiple risk factors remain matters for further study. Treatment of specific suicidal risk in patients with bipolar disorder must therefore also incorporate broader interventions based on the individual’s specific risk factors. 165 Such an approach would include societal interventions like means restriction 166 and a number of empirically tested suicide focused psychotherapy treatments. 167 168 Unfortunately, the availability of appropriate training, expertise, and care models for such treatments remains limited, even in higher income countries. 169
More scalable solutions, such as the deployment of shortened interventions via digital means could help to overcome this implementation gap; however, the effectiveness of such approaches cannot be assumed and requires empirical testing. For example, a recent large scale randomized controlled trial of an abbreviated online dialectical behavioral therapy skills training program was paradoxically associated with slightly increased risk of self-harm. 170
Treatment consideration in BD-II and bipolar spectrum conditions
Because people with BD-II primarily experience depressive symptoms and appear less likely to switch mood states compared with individuals with BD-I, 50 171 there has been a greater acceptance of the use of antidepressants in BD-II depression, including as monotherapy. 172 However, caution should be exercised when considering the use of antidepressants without a mood stabilizer in patients with BD-II who might also experience high rates of mood instability and rapid cycling. Such individuals can instead respond better to newer second generation antipsychotic agents such as quetiapine 173 and lumateperone, 93 which are supported by post hoc analyses of these more recent clinical trials with more BD-II patients. In addition, despite the absence of randomized controlled trials, open label studies have suggested that lithium and other mood stabilizers can have similar efficacy in BD-II, especially in the case of lamotrigine. 174
Psychotherapeutic approaches such as psychoeducation, cognitive behavioral therapy, and interpersonal and social rhythm therapy have been found to be helpful 115 and can be considered as the primary form of treatment for BD-II in some patients, although in most clinical scenarios BD-II is likely to occur in conjunction with psychopharmacology. While it can be tempting to consider BD-II a milder variant of BD-I, high rates of comorbid disorders, rapid cycling, and adverse consequences such as suicide attempts 175 176 highlight the need for clinical caution and the provision of multimodal treatment, focusing on mood improvement, emotional regulation, and better psychosocial functioning.
Precision medicine: can it be applied to improve the care of bipolar disorder?
The recent focus on precision medicine approaches to psychiatric disorders seeks to identify clinically relevant heterogeneity and identify characteristics at the level of the individual or subgroup that can be leveraged to identify and target more efficacious treatments. 1 177 178
The utility of such an approach was originally shown in oncology, where a subset of tumors had gene expression or DNA mutation signatures that could predict response to treatments specifically designed to target the aberrant molecular pathway. 179 While much of the emphasis of precision medicine has been on the eventual identification of biomarkers utilizing high throughput approaches (genetics and other “omics” based measurements), the concept of precision medicine is arguably much broader, encompassing improvements in measurement, potentially through the deployment of digital tools, as well as better conceptualization of contextual, cultural, and socioeconomic mechanisms associated with psychopathology. 180 181 Ultimately, the goal of precision psychiatry is to identify and target driving mechanisms, be they molecular, physiological, or psychosocial in nature. As such, precision psychiatry seeks what researchers and clinicians have often sought: to identify clinically relevant heterogeneity to improve prediction of outcomes and increase the likelihood of therapeutic success. The novelty being not so much the goals of the overarching approach, but the increasing availability of large samples, novel digital tools, analytical advances, and an increasing armamentarium of biological measurements that can be deployed at scale. 177
Although not unique to bipolar disorder, several clinical decision points along the life course of bipolar disorder would benefit from a precision medicine approach. For example, making an early diagnosis is often not possible based on clinical symptoms alone, since such symptoms are usually non-specific. A precision medicine approach could also be particularly relevant in helping to identify subsets of patients for whom the use of antidepressants could be beneficial or harmful. Admittedly, precision medicine approaches to bipolar disorder are still in their infancy, and larger, clinically relevant, longitudinal, and reliable phenotypes are needed to provide the infrastructure for precision medicine approaches. Such data remain challenging to obtain at scale, leading to renewed efforts to utilize the extant clinical infrastructure and electronic medical records to help emulate traditional longitudinal analyses. Electronic medical records can help provide such data, but challenges such as missingness, limited quality control, and potential biases in care 182 need to be resolved with carefully considered analytical designs. 183
Emerging treatments
Two novel atypical antipsychotics, amilsupride and bifeprunox, are currently being tested in phase 3 trials ( NCT05169710 and NCT00134459 ) and could gain approval for bipolar depression in the near future if these pivotal trials show a significant antidepressant effect. These drugs could offer advantages such as greater antidepressant effects, fewer side effects, and better long term tolerability, but these assumptions must be tested empirically. Other near term possibilities include novel rapid antidepressant treatments, such as (es)ketamine that putatively targets the glutamatergic system, and has been recently approved for treatment resistant depression, but which have not yet been tested in phase 3 studies in bipolar depression. Small studies have shown comparable effects of intravenous ketamine, 149 184 in bipolar depression with no short term evidence of increased mood switching or mood instability. Larger phase 2 studies ( NCT05004896 ) are being conducted which will need to be followed by larger phase 3 studies. Other therapies targeting the glutamatergic system have generally failed phase 3 trials in treatment resistant depression, making them unlikely to be tested in bipolar depression. One exception could be the combination of dextromethorphan and its pharmacokinetic (CYP2D6) inhibitor bupropion, which was recently approved for treatment resistant depression but has yet to be tested in bipolar depression. Similarly, the novel GABAergic compound zuranolone is currently being evaluated by the FDA for the treatment of major depressive disorder and could also be subsequently studied in bipolar depression.
Unfortunately, given the general efficacy for most patients of available treatments, few scientific and financial incentives exist to perform large scale studies of novel treatment in mania. Encouraging results have been seen in small studies of mania with the selective estrogen receptor modulator 185 tamoxifen and its active metabolite endoxifen, both of which are hypothesized to inhibit protein kinase C, a potential mechanistic target of lithium treatment. These studies remain small, however, and anti-estrogenic side effects have potentially dulled interest in performing larger studies.
Finally, several compounds targeting alternative pathophysiological mechanisms implicated in bipolar disorder have been trialed in phase 2 academic studies. The most studied has been N -acetylcysteine, a putative mitochondrial modulator, which initially showed promising results only to be followed by null findings in larger more recent studies. 186 Similarly, although small initial studies of anti-inflammatory agents provided impetus for further study, subsequent phase 2 studies of the non-steroidal agent celecoxib, 187 the anti-inflammatory antibiotic minocycline, 187 and the antibody infliximab (a tumor necrosis factor antagonist) 188 have not shown efficacy for bipolar depression. Secondary analyses have suggested that specific anti-inflammatory agents might be effective only for a subset of patients, such as those with elevated markers of inflammation or a history of childhood adversity 189 ; however, such hypotheses must be confirmed in adequately powered independent studies.
Several international guidelines for the treatment of bipolar disorder have been published in the past decade, 102 190 191 192 providing a list of recommended treatments with efficacy in at least one large randomized controlled trial. Since effect sizes tend to be moderate and broadly comparable across classes, all guidelines allow for significant choice among first line agents, acknowledging that clinical characteristics, such as history of response or tolerability, severity of symptoms, presence of mixed features, or rapid cycling can sometimes over-ride guideline recommendations. For acute mania requiring rapid treatment, all guidelines prioritize the use of second generation antipsychotics such as aripiprazole, quetiapine, risperidone, asenapine, and cariprazine. 102 192 193 Combination treatment is considered based on symptom severity, tolerability, and patient choice, with most guidelines recommending lithium or divalproate along with a second generation antipsychotic for mania with psychosis, severe agitation, or prominent mixed symptoms. While effective, haloperidol is usually considered a second choice option owing to its propensity to cause extrapyramidal symptoms. 102 192 193 Uniformly, all guidelines agree on the need to taper antidepressants in manic or mixed episodes.
For maintenance treatment, guidelines are generally consistent in recommending lithium if tolerated and without relative contraindications, such as baseline renal disease. 194 The second most recommended maintenance treatment is quetiapine, followed by aripiprazole for patients with prominent manic episodes and lamotrigine for patients with predominant depressive episodes. 194 Most guidelines recommend considering prophylactic properties when initially choosing treatment for acute manic episodes, although others suggests that acute maintenance treatments can be cross tapered with maintenance medications after several months of full reponse. 193
For bipolar depression, recent guidelines recommend specific second generation antipsychotics such as quetiapine, lurasidone, and cariprazine 102 192 193 For more moderate symptoms, consideration is given to first using lamotrigine and lithium. Guidelines remain cautious about the use of antidepressants (selective serotonin reuptake inhibitors, venlafaxine, or bupropion) in patients with BP-I, restricting them to second or third line treatments and always in the context of an anti-manic agent. However, for patients with BP-II and no rapid cycling, several guidelines allow for the use of carefully monitored antidepressant monotherapy.
Bipolar disorder is a highly recognizable syndrome with many effective treatment options, including the longstanding gold standard therapy lithium. However, a significant proportion of patients do not respond well to current treatments, leading to negative consequences, poor quality of life, and potentially shortened lifespan. Several novel treatments are being developed but limited knowledge of the biology of bipolar disorder remains a major challenge for novel drug discovery. Hope remains that the insights of genetics, neuroimaging, and other investigative modalities could soon be able to inform the development of rational treatments aimed to mitigate the underlying pathophysiology associated with bipolar disorder. At the same time, however, efforts are needed to bridge the implementation gap and provide truly innovative and integrative care for patients with bipolar disorder. 195 Owing to the complexity of bipolar disorder, few patients can be said to be receiving optimized care across the various domains of mental health that are affected in those with bipolar disorder. Fortunately, the need for improvement is now well documented, 196 and concerted efforts at the scale necessary to be truly innovative and integrative are now on the horizon.
Questions for future research
Among adolescents and young adults who manifest common mental disorders such as anxiety or depressive or attentional disorders, who will be at high risk for developing bipolar disorder?
Can we predict the outcomes for patients following a first manic or hypomanic episode? This will help to inform who will require lifelong treatment and who can be tapered off medications after sustained recovery.
Are there reliable clinical features and biomarkers that can sufficiently predict response to specific medications or classes of medication?
What are the long term consequences of lifelong treatments with the major classes of medications used in bipolar disorder? Can we predict and prevent medical morbidity caused by medications?
Can we understand in a mechanistic manner the pathophysiological processes that lead to abnormal mood states in bipolar disorder?
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: FSG performed the planning, conduct, and reporting of the work described in the article. FSG accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Competing interests: I have read and understood the BMJ policy on declaration of interests and declare no conflicts of interest.
Patient involvement: FSG discussed of the manuscript, its main points, and potential missing points with three patients in his practice who have lived with longstanding bipolar disorder. These additional viewpoints were incorporated during the drafting of the manuscript.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ . Falret’s discovery: the origin of the concept of bipolar affective illness. Translated by M. J. Sedler and Eric C. Dessain. Am J Psychiatry 1983;140:1127-33. doi: 10.1176/ajp.140.9.1127 OpenUrl CrossRef PubMed Web of Science
- ↵ Kraepelin E. Manic-depressive Insanity and Paranoia. Translated by R. Mary Barclay from the Eighth German. Edition of the ‘Textbook of Psychiatry.’ 1921.
- Merikangas KR ,
- Akiskal HS ,
- Koukopoulos A ,
- Jongsma HE ,
- Kirkbride JB ,
- Rowland TA ,
- Kessler RC ,
- Kazdin AE ,
- Aguilar-Gaxiola S ,
- WHO World Mental Health Survey collaborators
- Bergen SE ,
- Kuja-Halkola R ,
- Larsson H ,
- Lichtenstein P
- Smoller JW ,
- Lichtenstein P ,
- Sjölander A ,
- Mullins N ,
- Forstner AJ ,
- O’Connell KS ,
- Palmer DS ,
- Howrigan DP ,
- Chapman SB ,
- Pirooznia M ,
- Murray GK ,
- McGrath JJ ,
- Hickie IB ,
- ↵ Mostafavi H, Harpak A, Agarwal I, Conley D, Pritchard JK, Przeworski M. Variable prediction accuracy of polygenic scores within an ancestry group. Loos R, Eisen MB, O’Reilly P, eds. eLife 2020;9:e48376. doi: 10.7554/eLife.48376 OpenUrl CrossRef PubMed
- Westlye LT ,
- van Erp TGM ,
- Costa Rica/Colombia Consortium for Genetic Investigation of Bipolar Endophenotypes
- Pauling M ,
- ENIGMA Bipolar Disorder Working Group
- Schnack HG ,
- Ching CRK ,
- ENIGMA Bipolar Disorders Working Group
- Goltermann J ,
- Hermesdorf M ,
- Dannlowski U
- Gurholt TP ,
- Suckling J ,
- Lennox BR ,
- Bullmore ET
- Marangoni C ,
- Hernandez M ,
- Achtyes ED ,
- Agnew-Blais J ,
- Gilman SE ,
- Upthegrove R ,
- ↵ Etain B, Aas M. Childhood Maltreatment in Bipolar Disorders. In: Young AH, Juruena MF, eds. Bipolar Disorder: From Neuroscience to Treatment . Vol 48. Current Topics in Behavioral Neurosciences. Springer International Publishing; 2020:277-301. doi: 10.1007/7854_2020_149
- Johnson SL ,
- Weinberg BZS
- Stinson FS ,
- Costello CG
- Klein & Riso LP DN
- Sandstrom A ,
- Perroud N ,
- de Jonge P ,
- Bunting B ,
- Nierenberg AA
- Hantouche E ,
- Vannucchi G
- Zimmerman M ,
- Ruggero CJ ,
- Chelminski I ,
- Leverich GS ,
- McElroy S ,
- Mignogna KM ,
- Balling C ,
- Dalrymple K
- Kappelmann N ,
- Stokes PRA ,
- Jokinen T ,
- Baldessarini RJ ,
- Faedda GL ,
- Offidani E ,
- Viktorin A ,
- Launders N ,
- Osborn DPJ ,
- Roshanaei-Moghaddam B ,
- De Hert M ,
- Detraux J ,
- van Winkel R ,
- Lomholt LH ,
- Andersen DV ,
- Sejrsgaard-Jacobsen C ,
- Skjelstad DV ,
- Gregersen M ,
- Søndergaard A ,
- Brandt JM ,
- Van Meter AR ,
- Youngstrom EA ,
- Taylor RH ,
- Ulrichsen A ,
- Strawbridge R
- Hafeman DM ,
- Merranko J ,
- Hirschfeld RM ,
- Williams JB ,
- Spitzer RL ,
- Adolfsson R ,
- Benazzi F ,
- Regier DA ,
- Johnson KR ,
- Akinhanmi MO ,
- Biernacka JM ,
- Strakowski SM ,
- Goldberg JF ,
- Schettler PJ ,
- Coryell W ,
- Scheftner W ,
- Endicott J ,
- Zarate CA Jr . ,
- Matsuda Y ,
- Fountoulakis KN ,
- Zarate CA Jr .
- Bowden CL ,
- Brugger AM ,
- The Depakote Mania Study Group
- Calabrese JR ,
- Depakote ER Mania Study Group
- Weisler RH ,
- Kalali AH ,
- Ketter TA ,
- SPD417 Study Group
- Keck PE Jr . ,
- Cutler AJ ,
- Caffey EM Jr . ,
- Grossman F ,
- Eerdekens M ,
- Jacobs TG ,
- Grundy SL ,
- The Olanzipine HGGW Study Group
- Versiani M ,
- Ziprasidone in Mania Study Group
- Sanchez R ,
- Aripiprazole Study Group
- McIntyre RS ,
- Panagides J
- Calabrese J ,
- McElroy SL ,
- EMBOLDEN I (Trial 001) Investigators
- EMBOLDEN II (Trial D1447C00134) Investigators
- Lamictal 606 Study Group
- Lamictal 605 Study Group
- Keramatian K ,
- Chakrabarty T ,
- Nestsiarovich A ,
- Gaudiot CES ,
- Neijber A ,
- Hellqvist A ,
- Paulsson B ,
- Trial 144 Study Investigators
- Schwartz JH ,
- Szegedi A ,
- Cipriani A ,
- Salanti G ,
- Dorsey ER ,
- Rabbani A ,
- Gallagher SA ,
- Alexander GC
- Cerqueira RO ,
- Yatham LN ,
- Kennedy SH ,
- Parikh SV ,
- Højlund M ,
- Andersen K ,
- Correll CU ,
- Ostacher M ,
- Schlueter M ,
- Geddes JR ,
- Mojtabai R ,
- Nierenberg AA ,
- Goodwin GM ,
- Agomelatine Study Group
- Vázquez G ,
- Baldessarini RJ
- Altshuler LL ,
- Cuijpers P ,
- Miklowitz DJ ,
- Efthimiou O ,
- Furukawa TA ,
- Strawbridge R ,
- Tsapekos D ,
- Hodsoll J ,
- Vinberg M ,
- Kessing LV ,
- Forman JL ,
- Miskowiak KW
- Lewandowski KE ,
- Sperry SH ,
- Torrent C ,
- Bonnin C del M ,
- Martínez-Arán A ,
- Bonnín CM ,
- Tamura JK ,
- Carvalho IP ,
- Leanna LMW ,
- Karyotaki E ,
- Individual Patient Data Meta-Analyses for Depression (IPDMA-DE) Collaboration
- Vipulananthan V ,
- Hurlemann R ,
- UK ECT Review Group
- Haskett RF ,
- Mulsant B ,
- Trivedi MH ,
- Wisniewski SR ,
- Espinoza RT ,
- Vazquez GH ,
- McClintock SM ,
- Carpenter LL ,
- National Network of Depression Centers rTMS Task Group ,
- American Psychiatric Association Council on Research Task Force on Novel Biomarkers and Treatments
- Levkovitz Y ,
- Isserles M ,
- Padberg F ,
- Blumberger DM ,
- Vila-Rodriguez F ,
- Thorpe KE ,
- Williams NR ,
- Sudheimer KD ,
- Bentzley BS ,
- Konstantinou G ,
- Toscano E ,
- Husain MM ,
- McDonald WM ,
- International Consortium of Research in tDCS (ICRT)
- Sampaio-Junior B ,
- Tortella G ,
- Borrione L ,
- McAllister-Williams RH ,
- Gippert SM ,
- Switala C ,
- Bewernick BH ,
- Hidalgo-Mazzei D ,
- Mariani MG ,
- Fagiolini A ,
- Swartz HA ,
- Benedetti F ,
- Barbini B ,
- Fulgosi MC ,
- Burdick KE ,
- Diazgranados N ,
- Ibrahim L ,
- Brutsche NE ,
- Sinclair J ,
- Gerber-Werder R ,
- Miller JN ,
- Vázquez GH ,
- Franklin JC ,
- Ribeiro JD ,
- Turecki G ,
- Gunnell D ,
- Hansson C ,
- Pålsson E ,
- Runeson B ,
- Pallaskorpi S ,
- Suominen K ,
- Ketokivi M ,
- Hadzi-Pavlovic D ,
- Stanton C ,
- Lewitzka U ,
- Severus E ,
- Müller-Oerlinghausen B ,
- Rogers MP ,
- Li+ plus Investigators
- Manchia M ,
- Michel CA ,
- Auerbach RP
- Altavini CS ,
- Asciutti APR ,
- Solis ACO ,
- Casañas I Comabella C ,
- Riblet NBV ,
- Young-Xu Y ,
- Shortreed SM ,
- Rossom RC ,
- Amsterdam JD ,
- Brunswick DJ
- Gustafsson U ,
- Marangell LB ,
- Bernstein IH ,
- Karanti A ,
- Kardell M ,
- Collins FS ,
- Armstrong K ,
- Concato J ,
- Singer BH ,
- Ziegelstein RC
- ↵ Holmes JH, Beinlich J, Boland MR, et al. Why Is the Electronic Health Record So Challenging for Research and Clinical Care? Methods Inf Med 2021;60(1-02):32-48. doi: 10.1055/s-0041-1731784
- García Rodríguez LA ,
- Cantero OF ,
- Martinotti G ,
- Dell’Osso B ,
- Di Lorenzo G ,
- REAL-ESK Study Group
- Palacios J ,
- DelBello MP ,
- Husain MI ,
- Chaudhry IB ,
- Subramaniapillai M ,
- Jones BDM ,
- Daskalakis ZJ ,
- Carvalho AF ,
- ↵ Goodwin GM, Haddad PM, Ferrier IN, et al. Evidence-based guidelines for treating bipolar disorder: revised third edition Recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2016;30:495-553. doi: 10.1177/0269881116636545 OpenUrl CrossRef PubMed
- Verdolini N ,
- Del Matto L ,
- Regeer EJ ,
- Hoogendoorn AW ,
- Harris MG ,
- WHO World Mental Health Survey Collaborators
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Treating Bipolar Disorder Is Notoriously Difficult, but Research Underway Could Lead to New Options
- Review A Review of the Diagnosis, Treatment, and Prognosis of Bipolar Disorder Andrew A. Nierenberg, MD; Bruno Agustini, MD, PhD; Ole Köhler-Forsberg, MD, PhD; Cristina Cusin, MD; Douglas Katz, PhD; Louisa G. Sylvia, PhD; Amy Peters, PhD; Michael Berk, MD, PhD JAMA
When Major General Gregg Martin, PhD, MS, was a commander in the US Army, he was stressed. Very stressed. But soon, the anxiety of being on the battlefield turned into something unexpected: euphoria.
“I suddenly felt like I was Superman,” Martin recalled in an interview with JAMA. “I didn’t need sleep and had unbelievable energy; I was solving complex problems before anybody knew there was a problem to solve.”
The boost allowed him to excel at commanding his troops during the Iraq War. But it didn’t last.
Read More About
Suran M. Treating Bipolar Disorder Is Notoriously Difficult, but Research Underway Could Lead to New Options. JAMA. 2023;330(5):395–398. doi:10.1001/jama.2023.10057
Manage citations:
© 2024
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Digital Health
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Sexual Health
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatment
T r marques, g m goodwin.
- Author information
- Article notes
- Copyright and License information
Psychiatric Imaging Group, MRC London Institute of Medical Sciences, Hammersmith Hospital, Imperial College London, Du Cane Road, London W12 0NN, UK. E-mail: [email protected]
Received 2016 Jul 25; Revised 2016 Dec 10; Accepted 2017 Jan 9; Issue date 2017 May.
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
Bipolar affective disorder is a common neuropsychiatric disorder. Although its neurobiological underpinnings are incompletely understood, the dopamine hypothesis has been a key theory of the pathophysiology of both manic and depressive phases of the illness for over four decades. The increased use of antidopaminergics in the treatment of this disorder and new in vivo neuroimaging and post-mortem studies makes it timely to review this theory. To do this, we conducted a systematic search for post-mortem, pharmacological, functional magnetic resonance and molecular imaging studies of dopamine function in bipolar disorder. Converging findings from pharmacological and imaging studies support the hypothesis that a state of hyperdopaminergia, specifically elevations in D2/3 receptor availability and a hyperactive reward processing network, underlies mania. In bipolar depression imaging studies show increased dopamine transporter levels, but changes in other aspects of dopaminergic function are inconsistent. Puzzlingly, pharmacological evidence shows that both dopamine agonists and antidopaminergics can improve bipolar depressive symptoms and perhaps actions at other receptors may reconcile these findings. Tentatively, this evidence suggests a model where an elevation in striatal D2/3 receptor availability would lead to increased dopaminergic neurotransmission and mania, whilst increased striatal dopamine transporter (DAT) levels would lead to reduced dopaminergic function and depression. Thus, it can be speculated that a failure of dopamine receptor and transporter homoeostasis might underlie the pathophysiology of this disorder. The limitations of this model include its reliance on pharmacological evidence, as these studies could potentially affect other monoamines, and the scarcity of imaging evidence on dopaminergic function. This model, if confirmed, has implications for developing new treatment strategies such as reducing the dopamine synthesis and/or release in mania and DAT blockade in bipolar depression.
Introduction
Bipolar disorder (BD) is a severe mental illness characterised by recurrent episodes of mania, depression or mixed states. 1 , 2 The lifetime prevalence of the full spectrum of bipolar disorder is estimated to be 2–4% in the general population and it is the sixth leading cause of disability worldwide. 3 , 4 , 5 , 6 The costs due to BD are immense, with annual direct healthcare costs in the USA of about $30 billion and indirect costs of >$120 billion. 7 , 8
Lithium has been the mainstay of maintenance treatment for BD for decades, together with valproate, an option that has emerged more recently. However their modes of action have not been well established. By contrast antidopaminergic drugs do have well-understood class action at D2/3 receptors and have long been used to treat acute manic episodes. However, as will be explained below, newer drugs (particularly olanzapine and quetiapine) have been shown to have antimanic and antidepressant actions in bipolar disorder together with long-term benefit in preventing relapse to either pole of the illness. 9 , 10 , 11 , 12 , 13 , 14 , 15 Although the newer drugs were introduced for the treatment of schizophrenia, they have arguably represented a bigger advance for the management of bipolar disorder.
Despite these advances in treatment, many patients continue to experience high levels of disability. 11 Furthermore drugs may be associated with significant side-effect burden and the risk of toxicity and/or teratogenicity in some instances. 16 , 17 , 18 Hence better understanding of pathophysiology and drug action appears necessary to improve the use of current treatments and develop better alternatives.
The dopamine hypothesis of BD dates back at least to the 1970s. 19 , 20 , 21 Early incarnations focused on mania, and the parallels between the behavioural consequences of amphetamine ingestion and the antimanic actions of antidopaminergic drugs. If hyperdopaminergia underlies the development of manic symptoms, then hypodopaminergia might underlie the depressive phase of the illness. Thus, opposite changes in dopaminergic function were hypothesised to underlie the opposing affective poles of the disorder. 19 , 20 , 21 This theory did not explain how hyper- or hypodopaminergia would arise and subsequent versions proposed an additional component to the hypothesis, where an intrinsic dysregulation in the homoeostatic regulation of dopaminergic function leads to cyclical changes in dopaminergic neurotransmission, 22 , 23 which would further distinguish the dopamine hypothesis of bipolar from theories of schizophrenia. 24 Thus, faulty homoeostatic mechanisms responding to hyperdopaminergia in the manic phase of the illness are proposed to result in an excessive reduction in dopaminergic function, rapidly leading to a hypodopaminergic state and depression. In turn a faulty regulatory response to hypodopaminergia leads, to a switch back to mania. 22 , 23 Implicit in this model is that a normalisation of dopaminergic function leads to remission and euthymia. Clearly, some kind of dysregulation must be required to account for the onset of episodes, but BD is also characterised by inter-episode mood instability. 25 Any satisfactory theory must account for the randomness of much bipolar experience as well as the cyclicity. As current antimanic antipsychotics are all dopamine D2 receptor blockers, their use for mania has long supported the involvement of dopamine in mania, but the increasing use of some antidopaminergic drugs to treat bipolar depression and as maintenance drugs makes it timely to review the dopamine hypothesis of BD. Furthermore, a number of new lines of evidence relevant to the role of dopamine, in particular from molecular and functional neuroimaging, have developed in recent years. Thus, we synthesize evidence from pharmacological, in vivo neuroimaging and post-mortem studies addressing the role of the dopamine system in BD and then consider the treatment and drug development implications.
Animal models and their implications for understanding the role of dopamine in bipolar disorder
Initial animal models of mania were based on amphetamine-induced hyperlocomotion, and it was shown that lithium reverses this behaviour. 26 , 27 Following this, a dopamine transporter (DAT) knockout rodent model was developed, and dopamine transporter blockers other than amphetamine (such as GBR12909 ) have been used. Both these approaches have been shown to induce manic-like behaviour, such as hyperlocomotion and increased exploration. 28 , 29 Subsequently, dopamine receptor stimulation using quinipirole (a dopamine agonist) was shown to induce manic-like behaviour. 30 Interestingly, mood stabilisers such as valproate and carbamazepine reversed these effects. 30 Recently, Sidor and colleagues demonstrated the impact of alterations in the regulation of circardian rhythm on dopaminergic activity and behaviour. 31 In this study, mice with a mutation in a circadian clock gene displayed a manic-like phenotype as measured by hyperlocomotion in the daytime. Moreover, hyperlocomotion was linked to an elevated daytime spike in ventral tegmental area (VTA) dopaminergic activity, as well as increased dopamine synthesis and tyrosine hydroxylase activity. 31 This was further validated using sustained optogenetic stimulation of the VTA, which also induced hyperlocomotion behaviour. 31 Taken together this evidence suggests that hyperdopaminergia, induced either by increased dopamine release, dopamine transporter blockade or dopamine receptor stimulation, results in a mania-like phenotype in rodents. In contrast, lesions in dopaminergic areas (such as the VTA and substantia nigra) induce depressive behaviour, such as learned helplessness. 32 Moreover, optogenetic stimulation of VTA dopaminergic neurons reverses depressive behaviour (as assessed using the forced swim test in chronically stressed animals). 33 These models thus provide evidence that hypodopaminergia may induce depressive-like behaviours and hyperdopaminergia may induce manic-like behaviour. Further research is needed to determine the key components of the dopaminergic circuit underlying this, particularly in relation to depressive behaviour.
Post-mortem studies on dopamine gene expression in bipolar disorder
Table 1 shows the post-mortem studies addressing dopaminergic gene expression in BD. Overall the most consistent findings come from studies on the D2 receptor expression, with two studies suggesting that the D2 receptor is upregulated in BD in the dorsolateral prefrontal cortex. 34 , 35 However, to date only four studies, 28 , 30 , 34 , 36 have been conducted, and only two focus on the same region (dorsolateral prefrontal cortex). Thus, this finding still requires replication in other brain regions to determine if there is regional specificity. The literature on other dopaminergic receptors is more limited, with only two studies on the D1 receptor 34 , 37 and one study on the D5 receptor. 38 Another issue for the post-mortem studies is that they are affected by several confounding factors such as medication status, post-mortem interval, substance abuse and cause of death. Antidopaminergic treatment has been shown to increase D2/3 receptor levels in animals, 39 and there is evidence this may also occur in schizophrenia. 40 This suggests that prior treatment could also have affected the D2/3 receptor findings in BD. Finally, data on phase-specific changes are difficult to characterise as clinical status at the time of death remains unknown. Despite these limitations, post-mortem data supports the notion that an abnormality within the dopaminergic pathways, in particular involving D2/3 receptors, might play a role in the pathogenesis of BD.
Table 1. Post-mortem studies assessing the role of dopamine in bipolar disorder.
Abbreviations: DAT, dopamine transporter; DLPFC, dorsolateral prefrontal cortex; PCR, polymerase chain reaction; RT-PCR, reverse transcription polymerase chain reaction.
In vivo imaging of dopamine
Dopamine in mania.
We have summarised the in vivo imaging studies of mania in Table 2 . Interestingly, patients with psychotic mania showed an elevated density of D2/3 receptors as measured by N-[ 11 C]-methylspiperone, when compared with healthy controls (HC) and non-psychotic mania patients, 41 , 42 although, as this tracer has significant affinity for 5HT2 receptors as well, 43 this finding requires replication with more selective tracers. Moreover, no significant difference in the striatal D2/3 density was noted in non-psychotic mania patients compared to HC. 44 These studies also explored the relationship between manic symptoms (as assessed using Young's Mania Rating Scale Score) and dopamine synthesis capacity and D2/3 density, finding no significant correlations between these variables in patients with mania. 41 , 44 , 45 However, in one of these studies D2/3 density was directly correlated with psychosis scores on the present state examination. 41 Taken together, these data suggest that psychotic symptoms in mania may be associated with dopaminergic abnormalities, although the same cannot be inferred in non-psychotic mania patients.
Table 2. In vivo imaging studies assessing dopamine in mania.
Abbreviations: YMRS, Young's Mania Rating Scale; ↔, no significant difference.
*Further details of scan and patient characteristics are given in the Supplementary Material .
Dopamine in euthymic BD
Two studies have assessed dopamine transporters in the euthymic state and are conflicting. Chang et al reported an upregulation of the dopamine transporter in drug naive euthymic bipolar patients, while Anand et al. observed a downregulation in a group consisting of both euthymic bipolar and bipolar depression patients. 46 , 47 Additionally, one study has assessed the vesicular monoamine transporter protein (VMAT-2), located in presynaptic neurons and involved in the storage of dopamine. There was an increase in VMAT-2 in the thalamus and dorsal brainstem, but no significant alteration in striatum, in currently euthymic patients with a history of psychotic mania compared with HC. 48 A positron emission tomography (PET) study using [ 11 C]-SCH23390 found decreased D1 density in the frontal cortex but not in the striatum of bipolar patients compared to HC, suggesting a regional difference in D1 receptor distribution ( Table 3 ). 49
Table 3. In vivo imaging studies assessing dopamine in the depressive and euthymic phase of bipolar disease.
Abbreviations: DAT, dopamine transporter; DVR, distribution volume ratio; HDRS, Hamilton Depression Rating Scale; YMRS, Young's Mania Rating Scale.
So far, only one PET study has assessed dopamine release in BD. This study used [ 123 I]-IBZM to measure dopamine receptor density and release after amphetamine challenge in patients in their euthymic phase of illness, and found no significant differences between patients and HC. 50
Dopamine in bipolar depression
There is a paucity of literature on dopamine release and post-synaptic dopamine receptor density. Findings on dopamine transporter density remains controversial, with one study showing an increase in bipolar depressive patients when compared with HC, whilst the others, which recruited both euthymic and depressed patients, noted a reduction ( Table 3 ). 21 , 26
Dopamine, reward processing and bipolar disorder: functional magnetic resonance imaging studies
Dopaminergic projections from the VTA to the ventral striatum (VS) (including nucleus accumbens) and prefrontal cortex have an important role in reward processing 51 , 52 and have also been implicated in the processing of other behaviourally salient stimuli. 53 , 54 The word 'reward' implies three related functional elements: a positive reinforcer for learning, movement towards a desired object and subjective/emotional choices. The brain processes underlying reinforcement and movement can be quantitatively assessed using specific behavioural tasks and single cell or optogenetic recording in animals. 55 Tasks that inform emotion per se are increasingly being performed in man but necessarily with less direct measures of neuronal activity.
Investigations in animals have shown that individual neurons signal reward-related information in the midbrain (substantia nigra and VTA), striatum, orbitofrontal cortex, amygdala and associated structures. Most dopamine neurons in the substantia nigra and VTA show brief, phasic responses that reflect the difference in value between received reward and predicted reward. The precise relationship between cell firing and function is still debated, but it would be misleading to think of dopamine neurotransmission simply in terms of a pleasure signal. 56 Changes in BOLD signal occur in the human nucleus accumbens, striatum and frontal cortex over a time course of seconds in response to anticipated reward. 57 Consistent with the animal literature, event-related functional magnetic resonance imaging (fMRI) reward paradigms have demonstrated robust activation of the ventral striatum in relation to both the anticipation and receipt of reward, 58 , 59 , 60 , 61 presumably related to dopaminergic neurotransmission. 57 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69
In BD several fMRI studies employing reward tasks support the existence of abnormal reward-related neural activity in the VS and frontal cortex (task paradigms and results for VS summarised in Supplementary Table 2 and Table 4 , respectively). 61 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 This provides another indirect line of evidence for a dopaminergic abnormality in this disorder. We discuss the evidence in relation to specific mood polarities below.
Table 4. Functional magnetic resonance imaging studies investigating bipolar patients vs healthy controls during monetary reward tasks.
Abbreviations: ACC, anterior cingulate cortex; BD(I/II), bipolar disorder (I/II); BDI, beck depression inventory; DLPFC, dorsolateral prefrontal cortex; DS, dorsal striatum; fMRI, functional magnetic resonance imaging; HC, healthy controls; HDRS, Hamilton Depression Rating Scale; MDD, major depressive disorder; MID, monetary incentive delay task; NOS, not otherwise specified; YMRS, Young Mania Rating Scale.
Results presented are restricted to ventral striatum (VS), which has been most consistently implicated in event-related fMRI reward tasks. Values given as mean (s.d.) unless stated otherwise.
Subject characteristics and reward feedback analysis contrasts are given in Supplementary Table 2 .
Bipolar mania
During cued reward anticipation Abler et al. reported that medicated manic patients had reduced activity to high- vs no-anticipated reward in the VTA, 70 owing to increased neural activity for no-reward-predicting cues in BD patients. Three studies using monetary reward tasks found no difference in VS activation to cued reward anticipation between patients and controls. 70 , 71 , 80 Two of these studies did, however, find elevated frontal cortex activity during reward anticipation in manic patients. 71 , 80 During reward feedback Abler et al. reported reduced activity in response to receipt of probabilistic rewards in the VS in BD compared with HC. 70 This finding has not been replicated in more recent studies in patients with current manic symptoms 71 or a recent manic episode. 80
Together, these studies suggest hyperactive neuronal activity in putatively dopaminergic circuits of the reward system in currently manic patients, particularly during cue-induced reward anticipation. The precise nature of this abnormality, however, remains uncertain.
Euthymic bipolar
Euthymic patients are of particular interest because they are at risk of mania. In these patients abnormalities in dopaminergic function would then indicate how vulnerability might be mediated. In medicated euthymic bipolar I patients, VS and prefrontal cortex activity to cued reward anticipation has been variously reported as increased, 76 , 77 and no different 72 , 74 compared with controls. During reward feedback VS activity in euthymic bipolar I patients has been reported as increased, 72 , 74 , 76 no different 75 , 77 and decreased (in euthymic and mildly depressed patients), 81 compared with controls. Reward feedback related activation in the frontal cortex has also variously been reported as elevated, 75 , 76 decreased (in euthymic and mildly depressed patients) 81 or no different 74 , 77 in bipolar I patients compared with controls. In euthymic bipolar II patients Caseras et al. reported elevated VS and prefrontal cortex activity for cued reward anticipation compared with controls. 72 This finding, however, was not replicated in a more recent study of medication-naive bipolar II patients, which instead reported reduced anticipation-related activity in the right dorsal striatum in patients. 82 Both studies reported no difference in VS activity during reward feedback in patients vs controls. Increased responses in the anticipatory phase of the monetary incentive delay task have been described in euthymic unipolar patients. 83 Careful comparison of unipolar with bipolar cases will be necessary to distinguish network dysfunction associated with (hypo)mania from that with depression. All such studies need to be adequately powered and preferably address pre-specified hypotheses, not always a standard observed in imaging studies.
In summary, the precise nature of the abnormality of reward-related activity in euthymic bipolar patients remains unclear. However, abnormalities of reward processing are probably not confined to the manic phase of the illness. Important differences in task structure and the post hoc choice of analysis contrasts between these studies may account for the inconsistencies and non-replication. Further studies are required to explore the suggested differences between euthymic bipolar I, bipolar II and unipolar disorder.
Bipolar depression
Three studies have compared monetary reward processing in medicated depressed bipolar I patients and HC. Only one study analysed activity during cued reward anticipation; it reported no difference in anticipation-related activity between patients and HC in VS or prefrontal cortex, although there was blunting in the anterior cingulate cortex in depressed patients (bipolar and unipolar). Neural activity related to outcome anticipation per se was increased in left ventrolateral prefrontal cortex in patients with bipolar-1 disorder, compared with healthy controls or patients with unipolar depressive disorder; it may represent a more generalised ‘arousal' response in the bipolar depressed group. 73 Ventral striatal and prefrontal activation during reward feedback in bipolar depressive patients has been reported both as similar to controls 73 , 79 and decreased. 78
Recent fMRI studies and meta-analyses have demonstrated blunted activation of the reward network in the ventral striatum and frontal cortex in schizophrenia, 84 , 85 , 86 as well as major depressive disorder and alcohol addiction. 84 In contrast, the fMRI findings in bipolar disorder summarised above do not provide consistent evidence for blunting. It may be important to consider only studies in the manic state, because depressed or even euthymic (often dysthymic) bipolar patients may well show blunting. 82 In mania there was increased frontal activation to reward anticipation in two out of three studies. If this finding is confirmed in further studies, including direct comparisons with patients with schizophrenia, it could point to a key difference in the reward network between mania and schizophrenia. To date a small number of studies have compared reward processing in bipolar disorder with schizophrenia 70 or major depressive disorder. 73 , 78 Of these, one study reported blunted VS activation in depressed patients diagnosed with bipolar disorder compared with major depressive disorder, at reward feedback. 78 Only one study compared reward processing in schizophrenia and manic patients with controls. 70 Patients with schizophrenia and healthy controls showed an activation in the VTA on expectation of monetary rewards and nucleus accumbens activation during receipt vs omission of rewards. Manic patients, however, showed reduced differential activation in the nucleus accumbens on receipt vs omission of rewards compared to the healthy control subjects. Taken together with the findings in the frontal cortex discussed above, this small study does suggest that in mania there is a deficit in prediction error processing not seen in schizophrenia. It may further imply bipolar disorder specific changes in dopaminergic function, although how much of the fMRI response is driven by disrupted dopaminergic function remains to be determined. Further studies investigating differences in reward processing between bipolar disorder and other psychotic and affective disorders, and across illness phases, will shed light on the reward processing abnormalities specific to bipolar disorder.
Pharmacological evidence
Dopaminergic manipulations and the induction of mania.
The role of dopaminergic abnormalities in BD has been extensively investigated using a variety of pharmacological approaches ( Table 5 ). Firstly, studies have shown that psychostimulants, particularly amphetamine, cause mania-like symptoms in healthy volunteers. 87 , 88 , 89 , 90 Further, there are several case series of manic and hypomanic episodes in Parkinson's disease patients treated with Levodopa. 91 , 92 , 93 Bromocriptine, another dopamine agonist, has also been shown to induce manic symptoms. 94 , 95 Similarly, an increased risk of hypomania/mania was observed in bipolar patients who received stimulant (methylphenidate, amphetamine or modafinil) augmentation for bipolar depression. 96 Secondly, pharmacological strategies to deplete tyrosine, a dopamine precursor, are known to reduce manic symptoms, although it remains to be established if this is specifically due to reducing dopamine levels. 97 , 98 Alpha-methyl-p-tyrosine, which induces dopamine depletion by inhibition of tyrosine hydroxylase, also attenuates mania-like symptom in bipolar patients. 99 , 100
Table 5. Summary of pharmacological evidence on dopamine dysfunction in the bipolar disorder.
Abbreviation: AMPT, alpha-methyl-p-tyrosine.
Dopaminergic manipulations and the induction of bipolar depression
Reserpine and tetrabenazine depletes synaptic dopamine by irreversibly inhibiting vesicular uptake of monoamines and has long been known to induce depression. 101 , 102 In addition, a high prevalence of depression is seen in patients with Parkinson's disease and this has been linked to loss of striatal dopaminergic innervation. 103 , 104 Finally, depletion of tyrosine has been shown to precipitate depressive symptoms in remitted patients with a history of major depressive disorder. 105 , 106
Modulation of the dopamine system and treatment of bipolar disorder
Antidopaminergic drugs in the treatment of mania.
Dopamine antagonists and partial agonists are increasingly used in the treatment of acute mania, bipolar depression and also as maintenance treatment. 107 , 108 , 109 , 110 Olanzapine, risperidone, quetiapine, aripiprazole, asenapine, ziprasidone and cariprazine have been approved by the Food and Drug Administration (FDA) as monotherapy for the treatment of acute mania. 111 Pertinently, a network meta-analysis of 68 randomised controlled trials (RCT), involving 16 073 participants, addressed the efficacy of different drugs in the treatment of acute mania. This showed that dopamine antagonists have larger effect sizes (Haloperidol (standardised mean difference (SMD) relative to placebo: −0.56 (95% CI −0.69 to −0.43)), risperidone (−0.50 (−0.63 to −0.38)), olanzapine (−0.43 (−0.54 to −0.32)) than mood stabilisers for the treatment of acute mania (lithium) (−0.37 (−0.63 to −0.11)), carbamazepine (–0.36 (–0.60 to −0.11)), valproate (–0.20 (–0.37 to −0.04)). 14
As the blockade of the dopamine D2/3 receptors is their common mechanism of action, 24 it is likely that reduced dopamine neurotransmission at least contributes to the clinical efficacy of these drugs. This assumption is supported by the greater efficacy of the cis- but not the trans-isomer of clopenthixol in the treatment of manic symptoms, 112 as the cis-isomer is a high affinity D2/3 receptor blocker while the trans-isomer has much lower affinity for D2/3 receptors. 44 , 112
Use of antidopaminergic in the maintenance phase
The FDA have approved olanzapine as monotherapy, quetiapine and ziprasidone as adjunctive therapy, and aripiprazole and risperidone long acting injections as both adjunctive and monotherapy for the maintenance treatment of BD. 111 Although lithium and valproate should be preferred, recent guidelines highlight that dopaminergic drugs have a place in maintenance treatment. 113
Action of non-D2/3 blocker mood stabilisers on dopamine pathways
Interestingly, it is possible that sodium valproate might exhibit antimanic effect through an action on the dopaminergic system. 44 , 45 In a study consisting of 13 manic patients, 2 weeks of sodium valproate was shown to decrease presynaptic dopamine synthesis capacity, 45 although this was not correlated with clinical improvement. Interestingly D2/3 density remained essentially unchanged after valproate treatment, 44 despite the reduction in dopamine synthesis capacity with valproate, which is anticipated to alter D2/3 availability. Taken together these two could either suggest valproate blocks the capacity of the D2 receptor to respond to reduced dopamine synthesis, or that the capacity of D2 receptors to respond is intrinsically impaired in bipolar disorder. Although both possibilities are speculative at this stage, the latter is particularly interesting as it suggests that a failure of D2 adaptation could contribute to the pathophysiology of bipolar disorder, making the dopamine system more vulnerable to dopamine transporter driven changes in presynaptic function.
Although the exact mechanism by which lithium acts remains unclear, it is known to modulate signalling pathways downstream of dopamine receptors. Preclinical studies have shown that lithium reverses dopamine dependent behaviour by acting through the protein kinase B (AKT)/glycogen synthase kinase 3 signalling cascade. 114 Furthermore, lithium acts on the adenyl cyclase and phospho-inositide, as well as protein kinase C pathways, which are part of the intracellular signalling pathway downstream of dopamine receptors. 115 In addition, micro-dialysis studies show a reduction in extracellular dopamine levels in lithium treated animals. 116 , 117 , 118 In summary, there is evidence to suggest that some non-D2/3 blocking mood stabilisers also act to reduce dopamine transmission, either through reducing presynaptic dopamine synthesis capacity in the case of sodium valproate, or post-synaptic dopaminergic signal transduction in the case of lithium. The degree to which these effects explain the therapeutic efficacy of these compounds remains to be determined.
Use of dopaminergic treatments for bipolar depression
Three double-blind placebo-controlled studies have shown that short-term use of pramipexole, a D2/D3 receptor agonist, is efficacious as an augmentation strategy for the treatment of bipolar depression and positive results have also been seen in other open-label studies. 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 Although there have not been any RCTs investigating the efficacy of methylphenidate or amphetamines in bipolar depression, the available open-label and naturalistic studies point towards a benefit of stimulants in a selected group of patients with drowsiness and fatigue. 128 , 129 , 130 , 131 Randomised controlled studies and open-label reports with other stimulant like agents such as modafinil and its R-enantiomer, armodafinil also indicate efficacy in bipolar depression although the development programme for armodafinil failed. 132 , 133 , 134 , 135 , 136 , 137 , 138 There is evidence to support the potential use of monoamine oxidase inhibitors such as tranylcypromine in bipolar depression. 139 , 140 It is speculated that tranylcypromine acts as dopamine releaser with about 1/10th the potency of amphetamine. 139 , 140 There are thus several lines of evidence suggesting that dopaminergic augmentation is beneficial in bipolar depression.
However, there is also evidence that dopamine antagonists are effective in the treatment of bipolar depression. 15 The FDA has approved the combination of olanzapine and fluoxetine, as well as monotherapy with quetiapine or lurasidone, for the treatment of acute bipolar depression. A recent meta-analysis of 24 placebo-controlled trails ( n =7307) revealed the following order of efficacy of drugs for the treatment of bipolar depression: olanzapine+fluoxetine⩾valproate>quetiapine>lurasidone>olanzapine, aripiprazole and carbamazepine. 141 The analysis is interesting in showing that antidopaminergics on their own have efficacy in bipolar depression.
The evidence thus suggests that both dopaminergic agonists and dopaminergic blockers, are effective in treating bipolar depression. This presents a paradox for understanding the role of dopamine in bipolar depression. However, actions at receptors other than dopamine ones may underlie the efficacy of the dopamine blockers. For example, as well as all being D2/3 receptor blockers, olanzapine and quetiapine are both relatively high affinity 5HT 2A antagonists, 142 whilst both lurasidone and aripiprazole have high affinity for 5HT 1A receptors. 142 , 143 Potentially supporting this explanation, there are no clinical trials reporting efficacy of pure D2/3 blockers in bipolar depression. Nevertheless, the doses used in the clinical trials correspond to the dose ranges associated with substantial dopamine D2/3 receptor occupancy, 24 so dopamine receptor blockade is certainly compatible with antidepressant efficacy. The final consideration is that there has been a relatively small number of good quality RCTs for antidopaminergic treatment in bipolar depression, certainly in comparison to studies in mania. Studies that can directly test the mechanism underlying the mode of action of these drugs and pramipexole would be of great interest.
Our main findings for bipolar mania are that (i) there is consistent pharmacological evidence, especially from treatment studies, to support the hypothesis that a state of hyperdopaminergia can lead to mania; (ii) imaging studies support this hypothesis, with several studies reporting elevations in D2/3 receptor availability in psychotic mania and fMRI imaging evidence that identifies hyperactivity of the reward circuit in mania. Dopamine synthesis and receptor density appear to remain unchanged, at least in non-psychotic mania patients compared with HC.
For bipolar depression (i) pharmacological evidence shows that dopamine agonists are potentially beneficial for bipolar depression, but the same seems true for dopamine blocking drugs; (ii) the imaging studies show replicated increases in dopamine transporter levels, but there is inconsistency and it is not clear if there are other alterations as well. Figure 1 summarises our main imaging findings for mania and depression.
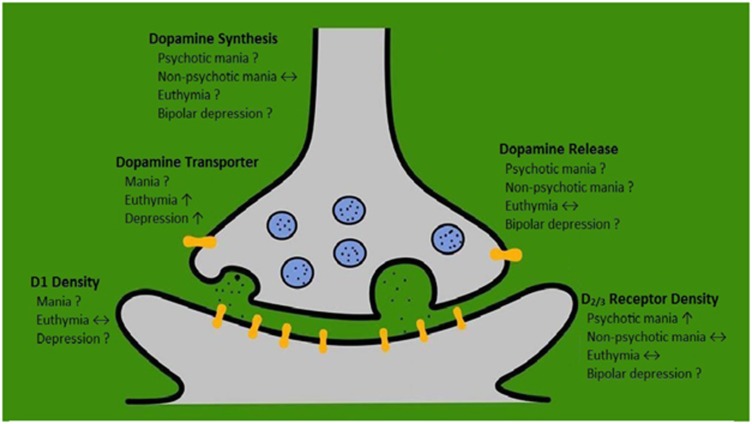
Summary of dopamine molecular imaging findings in bipolar disorder.
Finally, post-mortem evidence suggests an upregulation of the D2/3 receptors in bipolar patients, but interpretation is limited by lack of information on phase of illness and medication status at the time of death.
Implications for the dopamine hypothesis of bipolar disorder
More than four decades on from the early conceptualisations of the dopamine hypothesis of BD, it has stood the test of time, and the evidence for elements have strengthened. This is particularly the case for mania where the strength of the clinical trial evidence for the benefit of dopamine antagonists and partial agonists, supported by meta-analysis, would require an improbably large number of negative studies for reversal. Added to this there is now molecular and fMRI imaging evidence in bipolar disorder. Further, preclinical studies using optogenetic methods and knockout mice have shown that dopaminergic neuron activation leads to manic-like behaviour and it is linked to circadian gene expression. 31 , 144 Tentatively, these studies suggest elevated D2/3 receptor availability and a hyper-responsive reward system in ventral striatum in mania, and an increase in striatal dopamine transporter availability in bipolar depression. Dopamine neurotransmission in the striatum is primarily terminated by reuptake of dopamine into the presynaptic dopamine nerve terminal by dopamine transporters. Thus, an elevation in striatal D2/3 receptor availability in mania would lead to increased dopaminergic neurotransmission whilst increased striatal dopamine transporter levels in depression would lead to reduced dopaminergic function. This suggests a model in which elevated D2/3 receptor levels lead to altered reward processing and the development of mania, which is followed by a compensatory increase in dopamine transporter levels to reduce dopaminergic neurotransmission. However, if, over time, D2/3 receptor levels reduce but dopamine transporter levels do not normalise, this would then lead to reduced dopaminergic transmission, leading to depression and, in turn, a compensatory upregulation of D2/3 receptor levels, precipitating a further phase switch. One can see how a failure of homoeostatic regulation of the dopaminergic system could lead to cyclical periods of elevated and blunted dopaminergic neurotransmission. This model might apply most precisely to rapid cycling bipolar disorder. However it could be a component of all manic episodes, with other systems acting to disrupt the regular cyclicity that is so obvious in a substantial number of patients.
We recognise that this model is conjectural at this stage. Nevertheless, it makes predictions that can be tested empirically. In particular it predicts longitudinal changes in dopamine transporter and receptor levels linked to phase switches. Moreover it predicts that these changes and alterations in reward processing will pre-date symptom changes. However, many aspects of dopamine function in bipolar disorder are incompletely characterised. In particular baseline dopamine levels have not been measured in mania or depression. In addition, psychotic symptoms may also be present in manic patients, and psychosis per se may drive dopaminergic changes. 40 , 145 It is worth noting that, none of the studies have investigated dopamine function in mixed states. As approximately two thirds of depressed patients have concomitant manic symptoms, 146 any theory needs to explain mixed states as well as mania and depression. It would be hard to account for mixed states by dysfunction in dopaminergic function alone. Interestingly, asenapine seems to be more effective than olanzapine for mixed episodes. 147 As asenapine has higher affinity for 5HT2A than D2/3 receptors, which could suggest a role of serotonergic system in mixed episode states. Finally elevations in D 2/3 receptor availability would be predicted to increase dopaminergic neurotransmission via the indirect pathway, and reduce response to cues, 148 while the fMRI findings in mania do not seem to fit with this. However, the majority of the patients in these studies were treated with dopamine antagonists and mood stabilisers ( Supplementary Table 2 ), which confounds simple interpretation of effects based on dopamine neurotransmission.
Implications for treatment
If dopamine transmission is increased in mania, the use of D2/3 receptor blockers is logical, but alternative approaches, such as reducing dopamine synthesis and/or release, are alternative approaches that may be more effective and/or better tolerated if they could be sufficiently selective. Similarly, selective DAT blockade could be beneficial for BD depression, at the risk of precipitating mania. Finally mood stabilisation should improve homoeostatic regulation of dopaminergic neurotransmission, and this requires further evaluation and understanding.
Limitations and future directions
The key limitation of the dopamine hypothesis remains that its strongest supporting evidence comes from pharmacological studies, which offer an indirect and sometimes imprecise approach to studying dopaminergic function. Reserpine, alpha-methyl-para-tyrosine, amphetamine and l -DOPA, for example, can affect neurotransmission of other monoamines, in particular norepinephrine, which could contribute to the clinical effects observed. By the same token, the efficacy of antidopaminergic drugs in mania may be due to actions at other neurotransmitter systems, although relatively selective dopamine blockers do appear to be effective. There is a relative paucity of evidence from more direct measures, such as molecular imaging studies, and thus conclusions remain tentative at this stage. Earlier molecular imaging studies on D2/3 density in mania were conducted using non-selective ligand [ 11 C]N-methylspiperone, which has affinity to both D2/3 and 5HT2A receptors. 149 Interpretation is further complicated by some studies not being restricted to one illness phase. Moreover, none of the studies addressed dopamine transporter availability in mania, dopamine release in mania or dopamine release in bipolar depression (summarised in Figure 1).
Although our model suggests euthymia is a state of normalised dopamine, based on a study demonstrating no significant alteration in the dopamine release paradigm in euthymic patients compared to controls, 50 this is not consistent with the finding of elevated DAT in a euthymic state. 47 It also remains unclear whether the dopamine hypothesis can completely explain bipolar depression and how dopaminergic dysregulation will be linked to the involvement of other neurotransmitter systems.
A critical limitation is the lack of longitudinal studies that investigate changes across phases of illness, including mixed states. Ideally future studies should focus on elucidating phase-related dopamine dysfunction by studying patients longitudinally in euthymic, manic and depressive episodes to determine the direction of causality. Clearly this will be difficult, although a focus on rapid cycling patients might make it feasible. Cross-sectional studies are more feasible and could test key elements of the dopamine hypothesis if well designed. Another key issue is why some antidopaminergics are effective for bipolar depression. Molecular imaging studies are needed to determine whether dopaminergic, serotonergic or other systems are involved in their mode of action. Finally, although studies have found an effect of valproate and lithium on dopaminergic function, 44 , 115 it is not established if this is their mechanism of action. Determining whether dopaminergic mechanisms are common across classes of medication would be an important advance in understanding. Finally, it remains unclear if hyperdopaminergic activity is specific to mania or psychosis because many of the manic patients in the studies had psychotic symptoms as well. It is interesting to note that in schizophrenia molecular imaging studies indicate there is an elevation in dopamine synthesis and release capacity, but unaltered dopamine transporter and D2/3 receptor availability in striatum. 40 PET studies have also demonstrated elevated striatal dopamine turnover, but blunted cortical and midbrain dopamine release in schizophrenia. 150 In addition, blunting of the fMRI signal during reward tasks is observed in schizophrenia. 85 In contrast, studies in bipolar disorder suggest dopamine synthesis capacity is unaltered, at least in non-psychotic mania, but there is elevated D2/3 receptor availability in psychotic mania. However, direct comparisons of dopaminergic function in psychotic mania and schizophrenia as well as longitudinal studies of dopaminergic activity across various phases of illness are needed to determine if there are differences between mania and schizophrenia, and between mania and bipolar depression ( Box 1 ).
Future research direction.
Animal models exhibiting bipolar depression-like phenotype need to be developed.
Development of better animal models of mood polarity switching coupled with longitudinal, translational assays (such as PET, fMRI and behavioural methods).
Longitudinal molecular imaging studies investigating dopaminergic function, particularly dopamine transporter and D2/3 receptor homoeostasis, in patients across different illness phases.
Trans-diagnostic comparisons of dopaminergic function in psychotic and non-psychotic mania and schizophrenia.
Imaging studies in mixed states and rapid cycling bipolar disorder.
Longitudinal studies investigating the effects of antidopaminergic and conventional mood stabilisers on dopaminergic pathways and the relationship between dopaminergic blockade and treatment response in bipolar disorder.
Future studies should also focus on integration of data from molecular imaging studies with functional MRI to elucidate specific anatomical circuits involved and the link to molecular changes.
Molecular imaging studies should investigate extra-striatal dopaminergic changes across different phases of bipolar disorder.Abbreviations: fMRI, functional magnetic resonance imaging; PET, positron emission tomography.
Conclusions
The dopamine hypothesis of bipolar disorder proposes that faulty homoeostasis between dopamine transporter and receptors underlies depressive and manic phases of the illness. The available evidence suggests elevated D2/3 receptor availability and a hyper-responsive reward system in mania, and possibly increased dopamine transporter availability in bipolar depression. Future longitudinal studies are needed to elucidate the precise phase-related changes in dopaminergic function and the specificity of alterations to mania over psychosis.
Acknowledgments
AHA, TRM and MMN conduct research funded by the Medical Research Council (UK). TRM received honoraria as a speaker for Lundbeck. SJ conducts research funded by Medical Research Council (UK) and Wellcome trust. Professor Howes conducts research funded by the Medical Research Council (UK), the National Institute of Health Research (UK) and the Maudsley Charity. Professor Goodwin holds a grant from Wellcome Trust, holds shares in P1vital and has served as consultant, advisor or CME speaker for AstraZeneca, Merck, Cephalon/Teva, Eli Lilly, Lundbeck, Medscape, Otsuka, P1Vital, Pfizer, Servier, Sunovion, Takeda. He is a NIHR Senior Investigator. Professor Young has been a consultant to or has received honoraria or grants from AstraZeneca, Lunbeck, Eli Lilly, Janssen, Servier, Sunovion, Cyberonics and Wyeth. ODH has received investigator-initiated research funding from and/or participated in advisory/speaker meetings organised by AstraZeneca, BMS, Eli Lilly, Jansenn, Lundbeck, Lyden-Delta, Servier, and Roche. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
The authors declare no conflict of interest.
Supplementary Material
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA et al. Psychosocial disability in the course of bipolar I and II disorders: a prospective, comparative, longitudinal study. Arch Gen Psychiatry 2005; 62: 1322–1330. [ DOI ] [ PubMed ] [ Google Scholar ]
- Judd LL, Schettler PJ, Solomon DA, Maser JD, Coryell W, Endicott J et al. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J Affect Disord 2008; 108: 49–58. [ DOI ] [ PubMed ] [ Google Scholar ]
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2163–2196. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Merikangas KR, Cui L, Kattan G, Carlson GA, Youngstrom EA, Angst J. Mania with and without depression in a community sample of US adolescents. Arch Gen Psychiatry 2012; 69: 943–951. [ DOI ] [ PubMed ] [ Google Scholar ]
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry 2011; 68: 241–251. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet 2015; 387: 1561–1572. [ DOI ] [ PubMed ] [ Google Scholar ]
- Dilsaver SC. An estimate of the minimum economic burden of bipolar I and II disorders in the United States: 2009. J Affect Disord 2011; 129: 79–83. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jann MW. Diagnosis and treatment of bipolar disorders in adults: a review of the evidence on pharmacologic treatments. Am Health Drug Benefits 2014; 7: 489–499. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alda M. Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Mol Psychiatry 2015; 20: 661–670. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Geddes JR, Burgess S, Hawton K, Jamison K, Goodwin GM. Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials. Am J Psychiatry 2004; 161: 217–222. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gitlin M. Treatment-resistant bipolar disorder. Mol Psychiatry 2006; 11: 227–240. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ketter TA, Miller S, Dell'Osso B, Wang PW. Treatment of bipolar disorder: review of evidence regarding quetiapine and lithium. J Affect Disord 2016; 191: 256–273. [ DOI ] [ PubMed ] [ Google Scholar ]
- Severus E, Taylor MJ, Sauer C, Pfennig A, Ritter P, Bauer M et al. Lithium for prevention of mood episodes in bipolar disorders: systematic review and meta-analysis. Int J Bipolar Disord 2014; 2: 15. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cipriani A, Barbui C, Salanti G, Rendell J, Brown R, Stockton S et al. Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis. Lancet 2011; 378: 1306–1315. [ DOI ] [ PubMed ] [ Google Scholar ]
- Young AH, McElroy SL, Olausson B, Paulsson B. A randomised, placebo-controlled 52-week trial of continued quetiapine treatment in recently depressed patients with bipolar I and bipolar II disorder. World J Biol Psychiatry 2014; 15: 96–112. [ DOI ] [ PubMed ] [ Google Scholar ]
- Giles JJ, Bannigan JG. Teratogenic and developmental effects of lithium. Curr Pharm Des 2006; 12: 1531–1541. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gentile S. Lithium in pregnancy: the need to treat, the duty to ensure safety. Expert Opin Drug Saf 2012; 11: 425–437. [ DOI ] [ PubMed ] [ Google Scholar ]
- McKnight RF, Adida M, Budge K, Stockton S, Goodwin GM, Geddes JR. Lithium toxicity profile: a systematic review and meta-analysis. Lancet 2012; 379: 721–728. [ DOI ] [ PubMed ] [ Google Scholar ]
- Tissot R. The common pathophysiology of monaminergic psychoses: a new hypothesis. Neuropsychobiology 1975; 1: 243–260. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wittenborn JR. Deductive approaches to the catecholamine hypothesis of affective disorders. J Nerv Ment Dis 1974; 158: 320–324. [ DOI ] [ PubMed ] [ Google Scholar ]
- Singh MM. A unifying hypothesis on the biochemical basis of affective disorder. Psychiatr Q 1970; 44: 706–724. [ DOI ] [ PubMed ] [ Google Scholar ]
- Berk M, Dodd S, Kauer-Sant'anna M, Malhi GS, Bourin M, Kapczinski F et al. Dopamine dysregulation syndrome: implications for a dopamine hypothesis of bipolar disorder. Acta Psychiatr Scand Suppl 2007; (434): 41–49. [ DOI ] [ PubMed ]
- Cousins DA, Butts K, Young AH. The role of dopamine in bipolar disorder. Bipolar Disord 2009; 11: 787–806. [ DOI ] [ PubMed ] [ Google Scholar ]
- Howes OD, Egerton A, Allan V, McGuire P, Stokes P, Kapur S. Mechanisms underlying psychosis and antipsychotic treatment response in schizophrenia: insights from PET and SPECT imaging. Curr Pharm Des 2009; 15: 2550–2559. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harrison PJ, Cipriani A, Harmer CJ, Nobre AC, Saunders K, Goodwin GM et al. Innovative approaches to bipolar disorder and its treatment. Ann N Y Acad Sci 2016; 1366: 76–89. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berggren U, Tallstedt L, Ahlenius S, Engel J. The effect of lithium on amphetamine-induced locomotor stimulation. Psychopharmacology 1978; 59: 41–45. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gould TJ, Keith RA, Bhat RV. Differential sensitivity to lithium's reversal of amphetamine-induced open-field activity in two inbred strains of mice. Behav Brain Res 2001; 118: 95–105. [ DOI ] [ PubMed ] [ Google Scholar ]
- Perry W, Minassian A, Paulus MP, Young JW, Kincaid MJ, Ferguson EJ et al. A reverse-translational study of dysfunctional exploration in psychiatric disorders: from mice to men. Arch Gen Psychiatry 2009; 66: 1072–1080. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Young JW, Goey AK, Minassian A, Perry W, Paulus MP, Geyer MA. The mania-like exploratory profile in genetic dopamine transporter mouse models is diminished in a familiar environment and reinstated by subthreshold psychostimulant administration. Pharmacol Biochem Behav 2010; 96: 7–15. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shaldubina A, Einat H, Szechtman H, Shimon H, Belmaker RH. Preliminary evaluation of oral anticonvulsant treatment in the quinpirole model of bipolar disorder. J Neural Transm 2002; 109: 433–440. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sidor MM, Spencer SM, Dzirasa K, Parekh PK, Tye KM, Warden MR et al. Daytime spikes in dopaminergic activity drive rapid mood-cycling in mice. Mol Psychiatry 2015; 20: 1406–1419. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Winter C, von Rumohr A, Mundt A, Petrus D, Klein J, Lee T et al. Lesions of dopaminergic neurons in the substantia nigra pars compacta and in the ventral tegmental area enhance depressive-like behavior in rats. Behav Brain Res 2007; 184: 133–141. [ DOI ] [ PubMed ] [ Google Scholar ]
- Tye KM, Mirzabekov JJ, Warden MR, Ferenczi EA, Tsai HC, Finkelstein J et al. Dopamine neurons modulate neural encoding and expression of depression-related behaviour. Nature 2013; 493: 537–541. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kaalund SS, Newburn EN, Ye T, Tao R, Li C, Deep-Soboslay A et al. Contrasting changes in DRD1 and DRD2 splice variant expression in schizophrenia and affective disorders, and associations with SNPs in postmortem brain. Mol Psychiatry 2014; 19: 1258–1266. [ DOI ] [ PubMed ] [ Google Scholar ]
- Zhan L, Kerr JR, Lafuente MJ, Maclean A, Chibalina MV, Liu B et al. Altered expression and coregulation of dopamine signalling genes in schizophrenia and bipolar disorder. Neuropathol Appl Neurobiol 2011; 37: 206–219. [ DOI ] [ PubMed ] [ Google Scholar ]
- Glantz LA, Gilmore JH, Overstreet DH, Salimi K, Lieberman JA, Jarskog LF. Pro-apoptotic Par-4 and dopamine D2 receptor in temporal cortex in schizophrenia, bipolar disorder and major depression. Schizophr Res 2010; 118: 292–299. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pantazopoulos H, Stone D, Walsh J, Benes FM. Differences in the cellular distribution of D1 receptor mRNA in the hippocampus of bipolars and schizophrenics. Synapse 2004; 54: 147–155. [ DOI ] [ PubMed ] [ Google Scholar ]
- Knable MB, Barci BM, Webster MJ, Meador-Woodruff J, Torrey EF. Molecular abnormalities of the hippocampus in severe psychiatric illness: postmortem findings from the Stanley Neuropathology Consortium. Mol Psychiatry 2004; 9: 544. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ginovart N, Wilson AA, Hussey D, Houle S, Kapur S. D2-receptor upregulation is dependent upon temporal course of D2-occupancy: a longitudinal [11C]-raclopride PET study in cats. Neuropsychopharmacology 2009; 34: 662–671. [ DOI ] [ PubMed ] [ Google Scholar ]
- Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A et al. The nature of dopamine dysfunction in schizophrenia and what this means for treatment. Arch Gen Psychiatry 2012; 69: 776–786. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pearlson GD, Wong DF, Tune LE, Ross CA, Chase GA, Links JM et al. In vivo D2 dopamine receptor density in psychotic and nonpsychotic patients with bipolar disorder. Arch Gen Psychiatry 1995; 52: 471–477. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wong DF, Pearlson GD, Tune LE, Young LT, Meltzer CC, Dannals RF et al. Quantification of neuroreceptors in the living human brain: IV. Effect of aging and elevations of D2-like receptors in schizophrenia and bipolar illness. J Cereb Blood Flow Metab 1997; 17: 331–342. [ DOI ] [ PubMed ] [ Google Scholar ]
- Swart JA, van der Werf JF, Wiegman T, Paans AM, Vaalburg W, Korf J. In vivo binding of spiperone and N-methylspiperone to dopaminergic and serotonergic sites in the rat brain: multiple modeling and implications for PET scanning. J Cereb Blood Flow Metab 1990; 10: 297–306. [ DOI ] [ PubMed ] [ Google Scholar ]
- Yatham LN, Liddle PF, Lam RW, Shiah IS, Lane C, Stoessl AJ et al. PET study of the effects of valproate on dopamine D(2) receptors in neuroleptic- and mood-stabilizer-naive patients with nonpsychotic mania. Am J Psychiatry 2002; 159: 1718–1723. [ DOI ] [ PubMed ] [ Google Scholar ]
- Yatham LN, Liddle PF, Shiah IS, Lam RW, Ngan E, Scarrow G et al. PET study of [(18)F]6-fluoro-L-dopa uptake in neuroleptic- and mood-stabilizer-naive first-episode nonpsychotic mania: effects of treatment with divalproex sodium. Am J Psychiatry 2002; 159: 768–774. [ DOI ] [ PubMed ] [ Google Scholar ]
- Anand A, Barkay G, Dzemidzic M, Albrecht D, Karne H, Zheng QH et al. Striatal dopamine transporter availability in unmedicated bipolar disorder. Bipolar Disord 2011; 13: 406–413. [ DOI ] [ PubMed ] [ Google Scholar ]
- Chang TT, Yeh TL, Chiu NT, Chen PS, Huang HY, Yang YK et al. Higher striatal dopamine transporters in euthymic patients with bipolar disorder: a SPECT study with [Tc] TRODAT-1. Bipolar Disord 2010; 12: 102–106. [ DOI ] [ PubMed ] [ Google Scholar ]
- Zubieta JK, Huguelet P, Ohl LE, Koeppe RA, Kilbourn MR, Carr JM et al. High vesicular monoamine transporter binding in asymptomatic bipolar I disorder: sex differences and cognitive correlates. Am J Psychiatry 2000; 157: 1619–1628. [ DOI ] [ PubMed ] [ Google Scholar ]
- Suhara T, Nakayama K, Inoue O, Fukuda H, Shimizu M, Mori A et al. D1 dopamine receptor binding in mood disorders measured by positron emission tomography. Psychopharmacology 1992; 106: 14–18. [ DOI ] [ PubMed ] [ Google Scholar ]
- Anand A, Verhoeff P, Seneca N, Zoghbi SS, Seibyl JP, Charney DS et al. Brain SPECT imaging of amphetamine-induced dopamine release in euthymic bipolar disorder patients. Am J Psychiatry 2000; 157: 1108–1114. [ DOI ] [ PubMed ] [ Google Scholar ]
- Berridge KC. From prediction error to incentive salience: Mesolimbic computation of reward motivation. Eur J Neurosci 2012; 35: 1124–1143. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schultz W. Dopamine signals for reward value and risk: basic and recent data. Behav Brain Funct 2010; 6: 1–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Winton-Brown TT, Fusar-Poli P, Ungless MA, Howes OD. Dopaminergic basis of salience dysregulation in psychosis. Trends Neurosci 2014; 37: 85–94. [ DOI ] [ PubMed ] [ Google Scholar ]
- Howes OD, Nour MM. Dopamine and the aberrant salience hypothesis of schizophrenia. World Psychiatry 2016; 15: 3–4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tsai HC, Zhang F, Adamantidis A, Stuber GD, Bonci A, de Lecea L et al. Phasic firing in dopaminergic neurons is sufficient for behavioral conditioning. Science 2009; 324: 1080–1084. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schultz W. Updating dopamine reward signals. Curr Opin Neurobiol 2013; 23: 229–238. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schott BH, Minuzzi L, Krebs RM, Elmenhorst D, Lang M, Winz OH et al. Mesolimbic functional magnetic resonance imaging activations during reward anticipation correlate with reward-related ventral striatal dopamine release. J Neurosci 2008; 28: 14311–14319. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bartra O, McGuire JT, Kable JW. The valuation system: a coordinate-based meta-analysis of BOLD fMRI experiments examining neural correlates of subjectivevalue. NeuroImage 2013; 76: 412–427. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diekhof EK, Kaps L, Falkai P, Gruber O. The role of the human ventral striatum and the medial orbitofrontal cortex in the representation of reward magnitude - an activation likelihood estimation meta-analysis of neuroimaging studies of passive reward expectancy and outcome processing. Neuropsychologia 2012; 50: 1252–1266. [ DOI ] [ PubMed ] [ Google Scholar ]
- Liu X, Hairston J, Schrier M, Fan J. Common and distinct networks underlying reward valence and processing stages: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev 2011; 35: 1219–1236. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nusslock R, Young CB, Damme KSF. Elevated reward-related neural activation as a unique biological marker of bipolar disorder: assessment and treatment implications. Behav Res Therapy 2014; 62: 74–87. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aarts E, Roelofs A, Franke B, Rijpkema M, Fernandez G, Helmich RC et al. Striatal dopamine mediates the interface between motivational and cognitive control in humans: evidence from genetic imaging. Neuropsychopharmacology 2010; 35: 1943–1951. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dreher JC, Kohn P, Kolachana B, Weinberger DR, Berman KF. Variation in dopamine genes influences responsivity of the human reward system. Proc Natl Acad Sci USA 2009; 106: 617–622. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Forbes EE, Brown SM, Kimak M, Ferrell RE, Manuck SB, Hariri AR. Genetic variation in components of dopamine neurotransmission impacts ventral striatal reactivity associated with impulsivity. Mol Psychiatry 2009; 14: 60–70. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jonasson LS, Axelsson J, Riklund K, Braver TS, Ogren M, Backman L et al. Dopamine release in nucleus accumbens during rewarded task switching measured by [(1)(1)C]raclopride. NeuroImage 2014; 99: 357–364. [ DOI ] [ PubMed ] [ Google Scholar ]
- Schultz W. Multiple dopamine functions at different time courses. Annu Rev Neurosci 2007; 30: 259–288. [ DOI ] [ PubMed ] [ Google Scholar ]
- van der Schaaf ME, van Schouwenburg MR, Geurts DE, Schellekens AF, Buitelaar JK, Verkes RJ et al. Establishing the dopamine dependency of human striatal signals during reward and punishment reversal learning. Cereb Cortex 2014; 24: 633–642. [ DOI ] [ PubMed ] [ Google Scholar ]
- Knutson B, Gibbs SEB. Linking nucleus accumbens dopamine and blood oxygenation. Psychopharmacology 2007; 191: 813–822. [ DOI ] [ PubMed ] [ Google Scholar ]
- Pessiglione M, Seymour B, Flandin G, Dolan RJ, Frith CD. Dopamine-dependent prediction errors underpin reward-seeking behaviour in humans. Nature 2006; 442: 1042–1045. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Abler B, Greenhouse I, Ongur D, Walter H, Heckers S. Abnormal reward system activation in mania. Neuropsychopharmacology 2008; 33: 2217–2227. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bermpohl F, Kahnt T, Dalanay U, Hägele C, Sajonz B, Wegner T et al. Altered representation of expected value in the orbitofrontal cortex in Mania. Hum Brain Mapp 2010; 31: 958–969. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Caseras X, Lawrence NS, Murphy K, Wise RG, Phillips ML. Ventral striatum activity in response to reward: differences between bipolar i and II disorders. Am J Psychiatry 2013; 170: 533–541. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chase HW, Nusslock R, Almeida JR, Forbes EE, Labarbara EJ, Phillips ML. Dissociable patterns of abnormal frontal cortical activation during anticipation of an uncertain reward or loss in bipolar versus major depression. Bipolar Disord 2013; 15: 839–854. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dutra S, Cunningham W, Kober H, Gruber J. Elevated striatal reactivity across monetary and social rewards in bipolar I disorder. J Abnorm Psychol 2015; 124: 890–904. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Linke J, King AV, Rietschel M, Strohmaier J, Hennerici M, Gass A et al. Increased medial orbitofrontal and amygdala activation: evidence for a systems-level endophenotype of bipolar I disorder. Am J Psychiatry 2012; 169: 316–325. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mason L, O'Sullivan N, Montaldi D, Bentall RP, El-Deredy W. Decision-making and trait impulsivity in bipolar disorder are associated with reduced prefrontal regulation of striatal reward valuation. Brain 2014; 137: 2346–2355. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nusslock R, Almeida J, Forbes E, Versace A, Frank E, LeBarbara E et al. Waiting to win: elevated striatal and orbitofrontal cortical activity during reward anticipation in euthymic bipolar disorder adults. Bipolar Disord 2012; 14: 249–260. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Redlich R, Dohm K, Grotegerd D, Opel N, Zwitserlood P, Heindel W et al. Reward processing in unipolar and bipolar depression: a functional MRI study. Neuropsychopharmacology 2015; 40: 1–28. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Satterthwaite TD, Kable JW, Vandekar L, Katchmar N, Bassett DS, Baldassano CF et al. Common and dissociable dysfunction of the reward system in bipolar and unipolar depression reward dysfunction in depression. Neuropsychopharmacology 2015; 40: 1–11. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Singh MK, Chang KD, Kelley RG, Cui X, Sherdell L, Howe ME et al. Reward processing in adolescents with bipolar I disorder. J Am Acad Child Adolesc Psychiatry 2013; 52: 68–83. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Trost S, Diekhof EK, Zvonik K, Lewandowski M, Usher J, Keil M et al. Disturbed anterior prefrontal control of the mesolimbic reward system and increased impulsivity in bipolar disorder. Neuropsychopharmacology 2014; 39: 1914–1923. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yip SW, Worhunsky PD, Rogers RD, Goodwin GM. Hypoactivation of the ventral and dorsal striatum during reward and loss anticipation in antipsychotic and mood stabilizer-naive bipolar disorder. Neuropsychopharmacology 2015; 40: 658–666. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dichter GS, Kozink RV, McClernon FJ, Smoski MJ. Remitted major depression is characterized by reward network hyperactivation during reward anticipation and hypoactivation during reward outcomes. J Affect Disord 2012; 136: 1126–1134. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hagele C, Schlagenhauf F, Rapp M, Sterzer P, Beck A, Bermpohl F et al. Dimensional psychiatry: reward dysfunction and depressive mood across psychiatric disorders. Psychopharmacology 2015; 232: 331–341. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Radua J, Schmidt A, Borgwardt S, Heinz A, Schlagenhauf F, McGuire P et al. Ventral striatal activation during reward processing in psychosis: a neurofunctional meta-analysis. JAMA Psychiatry 2015; 72: 1243–1251. [ DOI ] [ PubMed ] [ Google Scholar ]
- Yan C, Yang T, Yu QJ, Jin Z, Cheung EF, Liu X et al. Rostral medial prefrontal dysfunctions and consummatory pleasure in schizophrenia: a meta-analysis of functional imaging studies. Psychiatry Res 2015; 231: 187–196. [ DOI ] [ PubMed ] [ Google Scholar ]
- Asghar SJ, Tanay VA, Baker GB, Greenshaw A, Silverstone PH. Relationship of plasma amphetamine levels to physiological, subjective, cognitive and biochemical measures in healthy volunteers. Hum Psychopharm 2003; 18: 291–299. [ DOI ] [ PubMed ] [ Google Scholar ]
- Silverstone T. Dopamine in manic depressive illness. A pharmacological synthesis. J Affect Disord 1985; 8: 225–231. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jacobs D, Silverstone T. Dextroamphetamine-induced arousal in human subjects as a model for mania. Psychol Med 1986; 16: 323–329. [ DOI ] [ PubMed ] [ Google Scholar ]
- Nurnberger JI Jr., Gershon ES, Simmons S, Ebert M, Kessler LR, Dibble ED et al. Behavioral, biochemical and neuroendocrine responses to amphetamine in normal twins and 'well-state' bipolar patients. Psychoneuroendocrinology 1982; 7: 163–176. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ko GN, Leckman JF, Heninger GR. Induction of rapid mood cycling during L-dopa treatment in a bipolar patient. Am J Psychiatry 1981; 138: 1624–1625. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harsch HH, Miller M, Young LD. Induction of mania by L-dopa in a nonbipolar patient. J Clin Psychopharmacol 1985; 5: 338–339. [ PubMed ] [ Google Scholar ]
- Murphy DL. L-dopa, behavioral activation and psychopathology. Res Publ Assoc Res Nerv Ment Dis 1972; 50: 472–493. [ PubMed ] [ Google Scholar ]
- Fisher G, Pelonero AL, Ferguson C. Mania precipitated by prednisone and bromocriptine. Gen Hosp Psychiatry 1991; 13: 345–346. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kemperman CJ, Zwanikken GJ. Psychiatric side effects of bromocriptine therapy for postpartum galactorrhoea. J R Soc Med 1987; 80: 387–388. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wingo AP, Ghaemi SN. Frequency of stimulant treatment and of stimulant-associated mania/hypomania in bipolar disorder patients. Psychopharmacol Bull 2008; 41: 37–47. [ PubMed ] [ Google Scholar ]
- McTavish SF, McPherson MH, Harmer CJ, Clark L, Sharp T, Goodwin GM et al. Antidopaminergic effects of dietary tyrosine depletion in healthy subjects and patients with manic illness. Br J Psychiatry 2001; 179: 356–360. [ DOI ] [ PubMed ] [ Google Scholar ]
- Scarna A, Gijsman HJ, McTavish SF, Harmer CJ, Cowen PJ, Goodwin GM. Effects of a branched-chain amino acid drink in mania. Br J Psychiatry 2003; 182: 210–213. [ DOI ] [ PubMed ] [ Google Scholar ]
- Anand A, Darnell A, Miller HL, Berman RM, Cappiello A, Oren DA et al. Effect of catecholamine depletion on lithium-induced long-term remission of bipolar disorder. Biol Psychiatry 1999; 45: 972–978. [ DOI ] [ PubMed ] [ Google Scholar ]
- van Enkhuizen J, Geyer MA, Halberstadt AL, Zhuang X, Young JW. Dopamine depletion attenuates some behavioral abnormalities in a hyperdopaminergic mouse model of bipolar disorder. J Affect Disord 2014; 155: 247–254. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schildkraut JJ. The catecholamine hypothesis of affective disorders: a review of supporting evidence. Am J Psychiatry 1965; 122: 509–522. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kenney C, Hunter C, Mejia N, Jankovic J. Is history of depression a contraindication to treatment with tetrabenazine? Clin Neuropharmacol 2006; 29: 259–264. [ DOI ] [ PubMed ] [ Google Scholar ]
- Martinez-Martin P, Damian J. Parkinson disease: depression and anxiety in Parkinson disease. Nat Rev Neurol 2010; 6: 243–245. [ DOI ] [ PubMed ] [ Google Scholar ]
- Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 2005; 128: 1314–1322. [ DOI ] [ PubMed ] [ Google Scholar ]
- Parker G, Brotchie H. Mood effects of the amino acids tryptophan and tyrosine: 'Food for Thought' III. Acta Psychiatr Scand 2011; 124: 417–426. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ruhe HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry 2007; 12: 331–359. [ DOI ] [ PubMed ] [ Google Scholar ]
- Greil W, Haberle A, Haueis P, Grohmann R, Russmann S. Pharmacotherapeutic trends in 2231 psychiatric inpatients with bipolar depression from the International AMSP Project between 1994 and 2009. J Affect Disord 2012; 136: 534–542. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hayes J, Prah P, Nazareth I, King M, Walters K, Petersen I et al. Prescribing trends in bipolar disorder: cohort study in the United Kingdom THIN primary care database 1995-2009. PloS One 2011; 6: e28725. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hooshmand F, Miller S, Dore J, Wang PW, Hill SJ, Portillo N et al. Trends in pharmacotherapy in patients referred to a bipolar specialty clinic, 2000-2011. J Affect Disord 2014; 155: 283–287. [ DOI ] [ PubMed ] [ Google Scholar ]
- Walpoth-Niederwanger M, Kemmler G, Grunze H, Weiss U, Hortnagl C, Strauss R et al. Treatment patterns in inpatients with bipolar disorder at a psychiatric university hospital over a 9-year period: focus on mood stabilizers. Int Clin Psychopharmacol 2012; 27: 256–266. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ketter TA, Miller S, Dell'Osso B, Calabrese JR, Frye MA, Citrome L. Balancing benefits and harms of treatments for acute bipolar depression. J Affect Disord 2014; 169: S24–S33. [ DOI ] [ PubMed ] [ Google Scholar ]
- Nolen WA. Dopamine and mania. The effects of trans- and cis-clopenthixol in a double-blind pilot study. J Affect Disord 1983; 5: 91–96. [ DOI ] [ PubMed ] [ Google Scholar ]
- Goodwin GM, Haddad PM, Ferrier IN, Aronson JK, Barnes T, Cipriani A et al. Evidence-based guidelines for treating bipolar disorder: Revised third edition recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2016; 30: 495–553. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Beaulieu JM, Sotnikova TD, Yao WD, Kockeritz L, Woodgett JR, Gainetdinov RR et al. Lithium antagonizes dopamine-dependent behaviors mediated by an AKT/glycogen synthase kinase 3 signaling cascade. Proc Natl Acad Sci USA 2004; 101: 5099–5104. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Malhi GS, Tanious M, Das P, Coulston CM, Berk M. Potential mechanisms of action of lithium in bipolar disorder. Current understanding. CNS Drugs 2013; 27: 135–153. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gambarana C, Ghiglieri O, Masi F, Scheggi S, Tagliamonte A, De Montis MG. The effects of long-term administration of rubidium or lithium on reactivity to stress and on dopamine output in the nucleus accumbens in rats. Brain Res 1999; 826: 200–209. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ichikawa J, Dai J, Meltzer HY. Lithium differs from anticonvulsant mood stabilizers in prefrontal cortical and accumbal dopamine release: role of 5-HT(1 A) receptor agonism. Brain Res 2005; 1049: 182–190. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ferrie LJ, Gartside SE, Martin KM, Young AH, McQuade R. Effect of chronic lithium treatment on D2/3 autoreceptor regulation of dopaminergic function in the rat. Pharmacol Biochem Behav 2008; 90: 218–225. [ DOI ] [ PubMed ] [ Google Scholar ]
- Burdick KE, Braga RJ, Nnadi CU, Shaya Y, Stearns WH, Malhotra AK. Placebo-controlled adjunctive trial of pramipexole in patients with bipolar disorder: targeting cognitive dysfunction. J Clin Psychiatry 2012; 73: 103–112. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cassano P, Lattanzi L, Soldani F, Navari S, Battistini G, Gemignani A et al. Pramipexole in treatment-resistant depression: an extended follow-up. Depress Anxiety 2004; 20: 131–138. [ DOI ] [ PubMed ] [ Google Scholar ]
- Dell'osso B, Timtim S, Hooshmand F, Miller S, Wang PW, Hill SJ et al. Superior chronic tolerability of adjunctive modafinil compared to pramipexole in treatment-resistant bipolar disorder. J Affect Disord 2013; 150: 130–135. [ DOI ] [ PubMed ] [ Google Scholar ]
- El-Mallakh RS, Penagaluri P, Kantamneni A, Gao Y, Roberts RJ. Long-term use of pramipexole in bipolar depression: a naturalistic retrospective chart review. Psychiatr Q 2010; 81: 207–213. [ DOI ] [ PubMed ] [ Google Scholar ]
- Goldberg JF, Burdick KE, Endick CJ. Preliminary randomized, double-blind, placebo-controlled trial of pramipexole added to mood stabilizers for treatment-resistant bipolar depression. Am J Psychiatry 2004; 161: 564–566. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lattanzi L, Dell'Osso L, Cassano P, Pini S, Rucci P, Houck PR et al. Pramipexole in treatment-resistant depression: a 16-week naturalistic study. Bipolar Disord 2002; 4: 307–314. [ DOI ] [ PubMed ] [ Google Scholar ]
- Perugi G, Toni C, Ruffolo G, Frare F, Akiskal H. Adjunctive dopamine agonists in treatment-resistant bipolar II depression: an open case series. Pharmacopsychiatry 2001; 34: 137–141. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sporn J, Ghaemi SN, Sambur MR, Rankin MA, Recht J, Sachs GS et al. Pramipexole augmentation in the treatment of unipolar and bipolar depression: a retrospective chart review. Ann Clin Psychiatry 2000; 12: 137–140. [ DOI ] [ PubMed ] [ Google Scholar ]
- Zarate CA Jr., Payne JL, Singh J, Quiroz JA, Luckenbaugh DA, Denicoff KD et al. Pramipexole for bipolar II depression: a placebo-controlled proof of conceptstudy. Biol Psychiatry 2004; 56: 54–60. [ DOI ] [ PubMed ] [ Google Scholar ]
- Carlson PJ, Merlock MC, Suppes T. Adjunctive stimulant use in patients with bipolar disorder: treatment of residual depression and sedation. Bipolar Disord 2004; 6: 416–420. [ DOI ] [ PubMed ] [ Google Scholar ]
- El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000; 2: 56–59. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lydon E, El-Mallakh RS. Naturalistic long-term use of methylphenidate in bipolar disorder. J Clin Psychopharmacol 2006; 26: 516–518. [ DOI ] [ PubMed ] [ Google Scholar ]
- Parker G, Brotchie H. Do the old psychostimulant drugs have a role in managing treatment-resistant depression? Acta Psychiatr Scand 2010; 121: 308–314. [ DOI ] [ PubMed ] [ Google Scholar ]
- Goss AJ, Kaser M, Costafreda SG, Sahakian BJ, Fu CH. Modafinil augmentation therapy in unipolar and bipolar depression: a systematic review and meta-analysis of randomized controlled trials. J Clin Psychiatry 2013; 74: 1101–1107. [ DOI ] [ PubMed ] [ Google Scholar ]
- Dell'Osso B, Ketter TA, Cremaschi L, Spagnolin G, Altamura AC. Assessing the roles of stimulants/stimulant-like drugs and dopamine-agonists in the treatment of bipolar depression. Curr Psychiatry Rep 2013; 15: 378. [ DOI ] [ PubMed ] [ Google Scholar ]
- Rao JS, Kellom M, Reese EA, Rapoport SI, Kim HW. Dysregulated glutamate and dopamine transporters in postmortem frontal cortex from bipolar and schizophrenic patients. J Affect Disord 2012; 136: 63–71. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] [ Retracted ]
- Lee FJ, Pei L, Liu F. Disruption of the dopamine transporter-dopamine D2 receptor interaction in schizophrenia. Synapse (New York, NY) 2009; 63: 710–712. [ DOI ] [ PubMed ] [ Google Scholar ]
- Amsterdam JD, Newberg AB. A preliminary study of dopamine transporter binding in bipolar and unipolar depressed patients and healthy controls. Neuropsychobiology 2007; 55: 167–170. [ DOI ] [ PubMed ] [ Google Scholar ]
- Nasr S. Modafinil as adjunctive therapy in depressed outpatients. Ann Clin Psychiatry 2004; 16: 133–138. [ DOI ] [ PubMed ] [ Google Scholar ]
- Nasr S, Wendt B, Steiner K. Absence of mood switch with and tolerance to modafinil: a replication study from a large private practice. J Affect Disord 2006; 95: 111–114. [ DOI ] [ PubMed ] [ Google Scholar ]
- Heijnen WT, De Fruyt J, Wierdsma AI, Sienaert P, Birkenhager TK. Efficacy of tranylcypromine in bipolar depression: a systematic review. J Clin Psychopharmacol 2015; 35: 700–705. [ DOI ] [ PubMed ] [ Google Scholar ]
- Shulman KI, Herrmann N, Walker SE. Current place of monoamine oxidase inhibitors in the treatment of depression. CNS Drugs 2013; 27: 789–797. [ DOI ] [ PubMed ] [ Google Scholar ]
- Selle V, Schalkwijk S, Vazquez GH, Baldessarini RJ. Treatments for acute bipolar depression: meta-analyses of placebo-controlled, monotherapy trials of anticonvulsants, lithium and antipsychotics. Pharmacopsychiatry 2014; 47: 43–52. [ DOI ] [ PubMed ] [ Google Scholar ]
- Farah A. Atypicality of atypical antipsychotics. Prim Care Companion J Clin Psychiatry 2005; 7: 268–274. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meyer JM, Loebel AD, Schweizer E. Lurasidone: a new drug in development for schizophrenia. Expert Opin Investig Drugs 2009; 18: 1715–1726. [ DOI ] [ PubMed ] [ Google Scholar ]
- Chung S, Lee EJ, Yun S, Choe HK, Park SB, Son HJ et al. Impact of circadian nuclear receptor REV-ERBalpha on midbrain dopamine production and mood regulation. Cell 2014; 157: 858–868. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fusar-Poli P, Howes OD, Allen P, Broome M, Valli I, Asselin MC et al. Abnormal prefrontal activation directly related to pre-synaptic striatal dopamine dysfunction in people at clinical high risk for psychosis. Mol Psychiatry 2011; 16: 67–75. [ DOI ] [ PubMed ] [ Google Scholar ]
- Goldberg JF, Perlis RH, Bowden CL, Thase ME, Miklowitz DJ, Marangell LB et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry 2009; 166: 173–181. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berk M, Tiller JW, Zhao J, Yatham LN, Malhi GS, Weiller E. Effects of asenapine in bipolar I patients meeting proxy criteria for moderate-to-severe mixed major depressive episodes: a post hoc analysis. J Clin Psychiatry 2015; 76: 728–734. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hazy TE, Frank MJ, O'Reilly RC. Neural mechanisms of acquired phasic dopamine responses in learning. Neurosci Biobehav Rev 2010; 34: 701–720. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hall H, Wedel I, Halldin C, Kopp J, Farde L. Comparison of the in vitro receptor binding properties of N-[3H]methylspiperone and [3H]raclopride to rat and human brain membranes. J Neurochem 1990; 55: 2048–2057. [ DOI ] [ PubMed ] [ Google Scholar ]
- Slifstein M, van de Giessen E, Van Snellenberg J, Thompson JL, Narendran R, Gil R et al. Deficits in prefrontal cortical and extrastriatal dopamine release in schizophrenia: a positron emission tomographic functional magnetic resonance imaging study. JAMA Psychiatry 2015; 72: 316–324. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- PDF (321.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
Key points. Worldwide, over 2.5% of the population will have either bipolar I or bipolar II during their lifetimes. These illnesses are associated with a greater than 10-year decrease in life span.
"This is an important step towards the kind of research into disease mechanisms that, across the history of medicine, has underwritten successful therapeutics." Big study, big effect. Bipolar disorder is a severe, heritable mood disorder that affects approximately 1 percent of people and often begins in early adulthood.
In 2023, the Heinz C. Prechter Bipolar Research Program was named as one of six institutions that is part of the BD² Integrated Network with BD²: Breakthrough Discoveries for Thriving with Bipolar Disorder.. Along with Brigham and Women's Hospital-McLean Hospital, University of California Los Angeles, Johns Hopkins University, Mayo Clinic, UTHealth Houston, the Prechter Program at the ...
Bipolar disorder is a mental health condition characterized by episodes of depression and mania that affects a person's mood, energy and ability to function in everyday life. As many as 70% of people with bipolar disorder are misdiagnosed at least once, according to research. These episodes can be disruptive and last for weeks to months.
These cohorts included individuals receiving clinical care for bipolar disorder and individuals classified as having bipolar disorder based on data from health registries, electronic health records, or repositories. The total combined sample included 41,917 individuals with bipolar disorder and 371,549 individuals without bipolar disorder.
Fewer than 50% of individuals find effective treatments. BD 2 was created to provide leadership to revitalize and expand the scientific field, implement fundamental direction for research, and offer new hope for those living with bipolar disorder. Researching previously unknown scientific foundations of bipolar disorder, including biological ...
Bipolar disorder is a mood disorder that includes at least one manic episode - characterized by elevated or agitated mood and often reduced need for sleep - accompanied by episodes of major ...
"Less than half of people with bipolar disorder describe themselves as having found effective treatments, meaning they've had a partial treatment response or intolerable side effects from medications," said Katherine E. Burdick, Ph.D., the Borus Distinguished Chair in Psychiatry and director of the Mood and Psychosis Research Program at Brigham and Women's Hospital.
Together with Harvard University, Stanford University, and the New York Genome Center, Yale will be one of four sites funded by $18 million in research grants from BD²: Breakthrough Discoveries for Thriving with Bipolar Disorder, a research funding initiative that brings together researchers, clinicians, philanthropists, and people with lived ...
Bipolar disorder is a heritable mental illness with complex etiology. We performed a genome-wide association study of 41,917 bipolar disorder cases and 371,549 controls of European ancestry, which ...
Bond came to Johns Hopkins last August from the University of Minnesota, where he was an associate professor of psychiatry and director of the university's Early-Stage Mood Disorders Program. His research interests lie in identifying biological and clinical factors to enable early, accurate diagnosis of bipolar disorder, and investigating the ...
Having bipolar disorder -- a serious mental illness that can cause both manic and depressed moods -- can make life more challenging. It also comes with a higher risk of dying early. Now, a study ...
This disorder is more common than bipolar I or II, especially in children and adolescents, and carries a similar risk for co-occurring psychiatric conditions, suicide attempts, and family history of bipolar disorder. Research also suggests that in patients with a family history of the illness, about half go on to develop bipolar I or II ...
Those insights could one day lead to new ways of treating the disorder that improve symptoms in many people, even those without the rare mutation. The researchers began by comparing the exomes, or protein-coding portion of the genome, of roughly 14,000 people with bipolar disorder to 14,000 healthy controls.
Bipolar Disorder News. Read the latest medical research on causes, symptoms and new treatments for bipolar disorder. ... Problems with our sleep and internal body clock can trigger or worsen a ...
Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a leading cause of disability and premature mortality.
February 26, 2016 • Science Update. Three types of symptoms emerged as powerful predictors of whether a youth with one parent with bipolar disorder will go on to develop the disorder, according to a new NIMH-funded study of 391 at-risk youth. January 28, 2016 • Science Update.
New Research on Treatment for Bipolar Depression. Johns Hopkins psychiatrists study whether unconventional transcranial magnetic stimulation (TMS) yields more rapid improvements for patients. Psychiatry researchers are embarking on a pilot study to learn if a novel form of transcranial magnetic stimulation (TMS) can yield more rapid ...
This Medical News article discusses the difficulties of studying, diagnosing, and treating bipolar disorder and new research initiatives to improve [Skip to Navigation] Our website uses cookies to enhance your experience.
In vivo imaging of dopamine Dopamine in mania. We have summarised the in vivo imaging studies of mania in Table 2.Interestingly, patients with psychotic mania showed an elevated density of D2/3 receptors as measured by N-[11 C]-methylspiperone, when compared with healthy controls (HC) and non-psychotic mania patients, 41, 42 although, as this tracer has significant affinity for 5HT2 receptors ...
Bipolar Disorder. In 2019, 40 million people experienced bipolar disorder (1). ... and research for mental health. WHO's Mental Health Gap Action Programme (mhGAP) uses evidence-based technical guidance, tools and training packages to expand services in countries, especially in resource-poor settings. ... F., van Ommeren, M., Flaxman, A ...
A new study, funded in part by the National Institute of Mental Health, showed that a new medication derived from ketamine is safe and acceptable for use in humans, setting the stage for clinical trials testing it for hard-to-treat mental disorders like severe depression.