- Study protocol
- Open access
- Published: 21 July 2021

Medical Assistance in Dying in patients with advanced cancer and their caregivers: a mixed methods longitudinal study protocol
- Madeline Li ORCID: orcid.org/0000-0002-3977-7437 1 , 2 na1 ,
- Gilla K. Shapiro ORCID: orcid.org/0000-0002-2214-8263 1 , 3 na1 ,
- Roberta Klein 1 ,
- Anne Barbeau 1 ,
- Anne Rydall ORCID: orcid.org/0000-0002-4692-9101 1 ,
- Jennifer A. H. Bell ORCID: orcid.org/0000-0003-3617-6852 1 , 2 , 4 ,
- Rinat Nissim ORCID: orcid.org/0000-0002-3624-5806 1 , 2 ,
- Sarah Hales ORCID: orcid.org/0000-0001-6404-8124 1 , 2 , 3 ,
- Camilla Zimmermann ORCID: orcid.org/0000-0003-4889-0244 1 , 2 , 3 , 5 ,
- Rebecca K. S. Wong 1 , 6 &
- Gary Rodin ORCID: orcid.org/0000-0002-6626-6974 1 , 2 , 3
BMC Palliative Care volume 20 , Article number: 117 ( 2021 ) Cite this article
7228 Accesses
6 Citations
7 Altmetric
Metrics details
The legal criteria for medical assistance in dying (MAiD) for adults with a grievous and irremediable medical condition were established in Canada in 2016. There has been concern that potentially reversible states of depression or demoralization may contribute to the desire for death (DD) and requests for MAiD. However, little is known about the emergence of the DD in patients, its impact on caregivers, and to what extent supportive care interventions affect the DD and requests for MAiD. The present observational study is designed to determine the prevalence, predictors, and experience of the DD, requests for MAiD and MAiD completion in patients with advanced or metastatic cancer and the impact of these outcomes on their primary caregivers.
A cohort of patients with advanced or metastatic solid tumour cancers and their primary caregivers will be recruited from a large tertiary cancer centre in Toronto, Ontario, Canada, to a longitudinal, mixed methods study. Participants will be assessed at baseline for diagnostic information, sociodemographic characteristics, medical history, quality of life, physical and psychological distress, attitudes about the DD and MAiD, communication with physicians, advance care planning, and use of psychosocial and palliative care interventions. Measures will subsequently be completed every six months and at the time of MAiD requests. Quantitative assessments will be supplemented by qualitative interviews in a subset of participants, selected using quota sampling methods.
This study has the potential to add importantly to our understanding of the prevalence and determinants of the DD, MAiD requests and completions in patients with advanced or metastatic cancer and of the experience of both patients and caregivers in this circumstance. The findings from this study may also assist healthcare providers in their conversations about MAiD and the DD with patients and caregivers, inform healthcare providers to ensure appropriate access to MAiD, and guide modifications being considered to broaden MAiD legislation and policy.
Peer Review reports
Following the decision of the Supreme Court of Canada on February 6, 2015 to decriminalize medical assistance in dying (MAiD), [ 1 ] the Federal Parliament of Canada passed Bill C-14 on June 17, 2016 to establish the legal eligibility criteria for MAiD. These criteria included the presence of a serious and incurable medical condition, an advanced state of irreversible decline in capability, enduring and intolerable physical or psychological suffering, and a reasonably foreseeable natural death [ 2 ]. Bill C-14 excluded mature minors or those with mental illness as the sole underlying medical condition. Legislative review of these criteria are now underway, and the passage of Bill C-7 on March 17, 2021 removed the requirements of a "reasonably foreseeable natural death" [ 3 , 4 ].
Over 21,500 people in Canada chose to end their lives through assisted dying in the first five years of MAiD, more than 67% of whom had advanced cancer [ 4 ]. The frequency of MAiD in Canada is increasing annually, [ 5 ] although the overall proportion of medically assisted deaths is in the middle of the international rates reported. These range from 0.3% of deaths in Oregon, United States, to 4.6% in the Netherlands [ 4 , 6 ]. In 2019, MAiD deaths in Canada represented approximately 2.5% of all deaths, [ 4 ] and 6.3% of cancer-related deaths [ 4 , 7 ]. Footnote 1
In 2007, we completed a longitudinal study of the desire for death (DD) in individuals with advanced cancer [ 8 ]. This early research confirmed that the DD occurs on a continuum from the passive wish that the end would come earlier than it would otherwise naturally occur, referred to as the desire for hastened death (DHD) or the wish to hasten death (WTHD), [ 9 , 10 , 11 ] to a more active desire to end life, reflected in requests for MAiD [ 12 ]. The DD is uncommon in patients with advanced cancer receiving active treatment, [ 8 ] but is reported in up to half of all individuals in palliative care, [ 13 , 14 , 15 ] and may paradoxically coexist with the will to live [ 16 ]. This paradox underlines the complexity of psychological states related to the DD and the importance of reflective conversations before action on such wishes is taken [ 17 ].
Research examining attitudes and correlates of the WTHD in patients with advanced cancer has largely been cross-sectional, retrospective or conducted in settings where assisted dying is not permitted [ 18 , 19 , 20 , 21 , 22 ]. In research conducted in palliative care settings, a transient WTHD was found in 11–55% of patients, while 3–20% reported a more pervasive and persistent wish to die [ 13 ]. In a Canadian survey of 377 cancer patients with a prognosis of less than six months, Wilson and colleagues [ 13 ] found that almost 70% reported no WTHD, more than 18% acknowledged a transient WTHD, and over 12% reported a clear and persistent WTHD on the Desire for Death Rating Scale [ 14 ]. These findings are consistent with our previous study in which more than 65% of patients with advanced cancer indicated they wanted to continue living regardless of the pain or suffering that their disease might cause, and only 1.2% reported a clear WTHD on the Schedule of Attitudes towards Hastened Death (≥10) [ 8 ]. This difference between the two studies is likely due to the Wilson study sampling patients closer to the end of life, whereas we studied ambulatory patients recruited from oncology clinics.
Studies have also found that the DD fluctuates widely over time, [ 8 , 14 , 23 , 24 ] even during the last two weeks of life [ 25 ]. In a sample of almost one thousand American patients with advanced disease, Emanuel and colleagues found that more than 10% reported seriously considering assisted death for themselves. However, on follow-up two to six months later, approximately half had changed their minds, and an almost equal number who had not initially been interested in assisted death were then considering it [ 26 ].
The DD in patients with advanced cancer may arise from a complex interaction of factors, such as the experience or fear of uncontrolled physical or psychological suffering, the wish to maintain a sense of personal autonomy, or the desire to avoid burdening others (Fig. 1 ) [ 27 , 28 ]. It has also been associated with pain, high disease burden, low self-esteem, poor spiritual well-being, attachment insecurity, being unmarried, younger age, and having a history of psychiatric illness [ 18 , 25 , 26 , 29 , 30 , 31 , 32 ]. Some of these factors, such as those related to self-esteem, spiritual well-being, and attachment security, may be modifiable through specific psychotherapies, such as Managing Cancer and Living Meaningfully, [ 33 ] a brief, supportive-expressive intervention developed by our team and now being delivered internationally. Attachment security refers to an individual’s expectations and preferences regarding support from significant others in times of need and the capacity to make use of such support to relieve distress [ 34 ]. A secure attachment style, reflecting comfort with closeness and reliance on others, has been shown to protect against depression in cancer patients [ 35 ]. An avoidant attachment style, characterized by inflexible self-reliance, the need for personal control, and reluctance to accept support from others, has been associated in cancer patients with problematic relationships with oncologists [ 36 ] and requests for assisted dying [ 30 , 37 ].

MAiD, Medical Assistance in Dying; WTHD, Wish to Hasten Death
Physical symptom burden has been found to predict the DD [ 8 , 26 , 29 ] in patients with advanced cancer, although the motivation for MAiD in those who request and receive it is more often related to the loss of meaning, autonomy, and identity [ 19 , 38 , 39 ]. Some studies have found that religious observance and religious denomination have been linked to attitudes about assisted dying [ 40 , 41 ]. The influence of social and demographic factors on MAiD requests also deserves further exploration. Research thus far indicates that MAiD completion is more common in those who are older, Caucasian, more highly educated, and more affluent [ 38 , 39 ].
Dramatic changes have occurred over the past decade in Canada and throughout the world in public attitudes and expectations about death and dying, in access to psychosocial and palliative care for cancer patients, and, most recently, in the availability of MAiD. These changes may increase the likelihood that individuals with advanced disease and their caregivers will reflect upon and communicate the DD, engage in advance care planning, or consider actions to end their lives. While patients who request MAiD most often have access to specialized palliative care in settings where this is available, [ 4 , 42 , 43 ] the extent to which early palliative and supportive care interventions and empathic communication with healthcare providers about the goals of care at the end of life can affect the DD and requests for MAiD is unknown. Further, although caregivers are likely to be affected by patients’ DD and MAiD requests, [ 44 , 45 , 46 , 47 , 48 , 49 ] there is only limited research evaluating their experiences and support needs in these circumstances [ 20 , 26 , 48 ].
Caregivers typically experience a dramatic change in their daily lives and roles following the diagnosis of cancer or advanced disease in a loved one, related to the loss of family income [ 48 ] and the requirements for practical, social, and emotional support [ 47 , 49 ]. They must often shoulder the physical and psychological burden of caregiving, while also facing the suffering and threat of mortality in their loved one, their own fear of facing the future alone, and the financial strain caused by the illness. Although decisions about assisted dying may have an impact on primary caregivers, we know relatively little about the impact of their distress on the emergence and persistence of the DD and MAiD requests in patients with advanced cancer [ 50 ]. Understanding the experience of caregivers in relation to MAiD is therefore an important area in need of further research.
Optimal end-of-life care for patients with advanced cancer requires healthcare providers to engage in conversations with those who express a DD and/or who request MAiD. Cross-sectional research has identified some factors associated with the DD and MAiD requests, but it is not possible from such studies to distinguish confounding from correlational and causal factors, or to determine the course of an individual’s desire for MAiD in the face of advanced cancer.
We will be conducting a longitudinal study to examine the prevalence, trajectory, predictors, and nature of the desire for MAiD in a geographic setting where MAiD is legally available. The goals of this mixed methods study are to estimate the prevalence of the DD in patients with advanced cancer; to understand the trajectory and contributors to the DD, MAiD requests and MAID completion; and to elucidate the experience and support needs of their primary caregivers. The findings of this study could inform the training of healthcare providers regarding conversations with patients with advanced cancer and their caregivers about goals of care at the end of life, the DD, and MAiD as well as psychotherapeutic conversations about the DD. This information will also support the review of legislation to ensure appropriate access to MAiD.
To determine in patients with advanced cancer:
The prevalence of the DD, MAiD requests, and MAiD completions.
The trajectory and predictors of the DD, MAiD requests, and MAiD completions.
To examine the predictors of distress in primary caregivers of patients with advanced cancer.
Study design
This research is a prospective, longitudinal, mixed methods study conducted with patients with advanced or metastatic cancer and their primary caregivers. This study was approved on September 2, 2020, by the University Health Network Research Ethics Board (UHN REB #18–6182), and all participants will provide informed consent. Any protocol amendments will be submitted to the UHN REB for approval, and important changes that could impact participants’ willingness to continue in the study will be communicated to them in a timely manner. Data collection is expected to begin by January 2021.
Participants and setting
We plan to retain a longitudinal cohort of 600 patients with advanced or metastatic cancer and 300 of their primary caregivers recruited from the outpatient medical oncology clinics at the Princess Margaret Cancer Centre (PM), University Health Network, in Toronto, Canada’s largest comprehensive cancer treatment, education and research centre. This sample size is required to test our proposed regression model for predictors of MAiD requests and completions (Fig. 1 ), in which we will need at least 110 patients with at least two data points (baseline and one follow-up) [ 8 ], based on five to ten observations required for each of the 11 predictors included in our SEM [ 51 ]. Given that MAiD accounts for almost 5% of cancer deaths, and this represents 26% of MAiD requests at PM [ 39 ], we estimate ~ 115 subjects requesting MAiD and ~ 30 subjects receiving MAiD among 600 recruited patients.
To accommodate an anticipated 25% drop-out rate, we will recruit 800 patients and 400 primary caregivers over approximately 3.5 years for a final sample size of 600 patients and 300 primary caregivers. This is feasible given that PM provides care for approximately, 3200 Stage III or IV cancer patients per year, 60% of whom are expected to meet inclusion criteria; a conservative estimate is that 50% will provide informed consent, yielding approximately 960 eligible and consenting participants per year.
Participant recruitment and eligibility
Patients will be included if they: 1) are age 18 years or older; 2) are able to speak and read English sufficiently well to provide informed consent and complete questionnaires and/or interviews; and 3) have been diagnosed with advanced or metastatic solid tumour cancers of any type. Exclusion criteria will include: 1) significant cognitive impairment documented in their medical record or indicated by a score of < 20 on the Short Orientation-Memory-Concentration Test (SOMC); and 2) lack of sufficient proficiency in the English language to provide informed consent and complete the questionnaires and/or interviews. Trained research personnel will conduct the informed consent discussion with eligible and interested patients. Eligible patients who decline to participate will be asked their permission to allow the research team to document basic demographics to allow for later assessment of generalizability. Participants who begin the study will be considered withdrawn if they are later unable to participate due to a deterioration in cognitive functioning or physical capacity.
Individuals identified by participants as their primary caregivers will be approached by research personnel for recruitment if they are: 1) age 18 years or older; and 2) able to speak and read English sufficiently well to provide informed consent and complete questionnaires and/or interviews. A primary caregiver may be the spouse or partner of the patient, a relative or other family member, or a close friend. Caregivers may continue to participate in this study even if the patient participant subsequently withdraws from the study.
Study measures
Questionnaire package.
At baseline, patients and caregivers will complete both sets of baseline-only and follow-up measures. All participants will provide sociodemographic information at baseline. The Short Orientation-Memory-Concentration Test (SOMC) [ 52 ] will be conducted with patients at baseline in order to test patient’s cognitive function; this measure may be repeated at follow-up at the discretion of the research assistant. See Tables 1 and 2 for a description of the key study measures listed below, and Fig. 2 for the schedule of participant assessments.
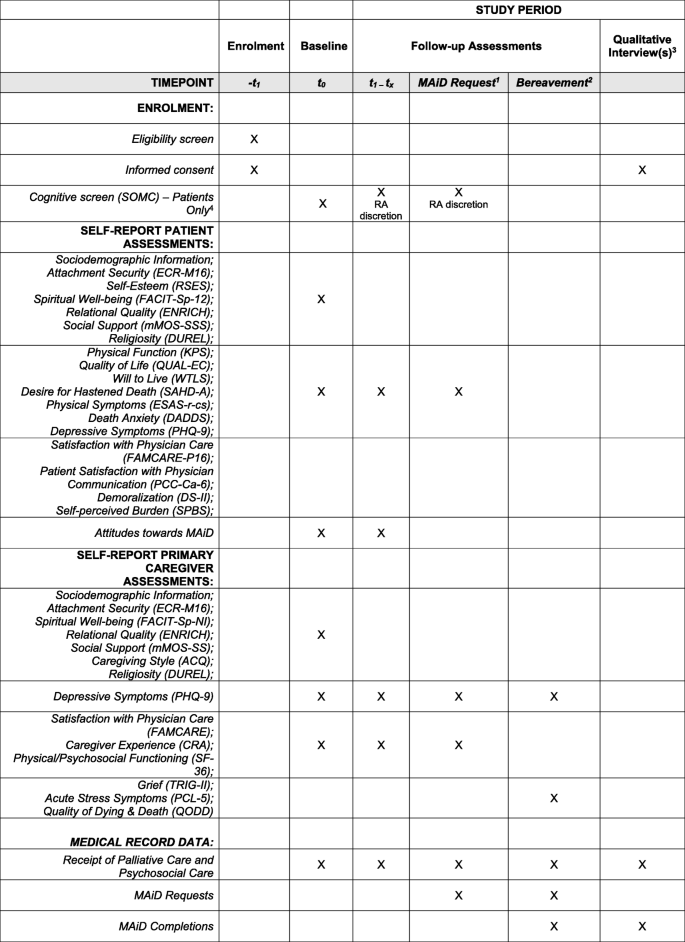
1 If a patient requests MAiD during the study, even if it falls between the 6 monthly scheduled time points, the patient and their primary caregiver (if applicable), will be invited to complete a follow-up assessment and a qualitative interview at this time. 2 In the event that a patient dies during the study (whether by MAiD or other causes), the patient’s primary caregiver (if applicable), will be approached within 6 months of the patient’s death to complete a final follow-up bereavement assessment and a qualitative interview. 3 In addition to qualitative interviews with patients requesting MAiD and their participating caregivers, and bereavement interviews with participating caregivers whose loved ones die during the study, a subset of participants (patients and caregivers) will be identified through purposeful sampling and invited to complete one or more qualitative interview(s) at the 6 monthly follow-up time points over the course of the study. 4 The SOMC may be re-administered at the discretion of the study research assistant if they feel the patient’s cognitive status may be impaired or have declined since the previous assessment. In the event that a patient fails a cognitive screen during the study, they will be withdrawn by the study principal investigator
Patient Baseline-Only Measures : Attachment Security: Brief Modified Experiences in Close Relationships scale (ECR-M16) [ 89 ]; Spiritual Well-being: Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being scale (FACIT-Sp-12, 58) Relational Quality: ENRICH Marital Satisfaction Scale (ENRICH) [ 74 ]; Social Support: The modified Medical Outcomes Study Social Support Survey (mMOS-SSS) [ 75 , 76 ]; Religiosity: The Duke University Religion Index (DUREL) [ 77 ]; and, Self-Esteem : The Rosenberg Self-Esteem Scale (RSES) [ 64 ].
Patient Baseline and Follow-up Measures: Physical Function: The Karnofsky Performance Status index (KPS) [ 53 , 54 ]; Quality of Life: The Quality of Life at the End of Life Scale-Cancer scale (QUAL-EC) [ 55 , 56 ]; Will to Live: The Will to Live Scale (WTLS) [ 57 ]; Desire for Hastened Death: The Schedule of Attitudes towards Hastened Death–Abbreviated (SAHD-A) [ 58 ]; Depressive Symptoms: Patient Health Questionnaire-9 (PHQ-9) [ 59 ]; Physical Symptoms: Edmonton Symptom Assessment System-Revised, including constipation and sleep disturbance (ESAS-r-cs) [ 60 , 61 , 62 ]; Death Anxiety: Death and Dying Distress Scale (DADDS) [ 65 , 66 , 67 ]; Patient Satisfaction with Physician Communication: Patient-Centered Communication-Cancer-6 items (PCC-Ca-6) [ 68 ]; Satisfaction with Physician Care: Modified FAMCARE Scale – Patient-16 items (FAMCARE-P16) [ 63 ]; Demoralization: Demoralization Scale-II (DS-II) [ 70 , 79 ]; and, Self-Perceived Burden: Self-Perceived Burden Scale (SPBS) [ 71 ]. Participants will also answer several questions to assess their attitudes towards MAiD.
Caregiver Baseline-Only Measures: Attachment Security: Brief Modified Experiences in Close Relationships scale (ECR-M16) [ 89 ]; Spiritual Well-being: Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being–Non-illness version (FACIT-Sp-NI) [ 72 , 73 ]; Relational Quality: ENRICH Marital Satisfaction Scale (ENRICH) [ 74 ]; Social Support: The modified Medical Outcomes Study Social Support Survey (mMOS-SSS) [ 75 , 76 ]; Caregiving Style: The Adult Caregiving Questionnaire [ 78 ]; Religiosity: The Duke University Religion Index (DUREL) [ 77 ].
Caregiver Baseline and Follow-up Measures: Depressive Symptoms: Patient Health Questionnaire-9 (PHQ-9) [ 59 ]; Satisfaction with Physician Care: FAMCARE Scale (FAMCARE) [ 69 ]; Caregiver Experience: The Caregiver Reaction Assessment scale [ 80 ]; Physical and Psychosocial Functioning: The Medical Outcomes Study Short-Form 36 (SF-36) [ 82 ].
We will also administer measures to caregivers six months post-patient death: Grief: The Texas Revised Inventory of Grief-Part II (TRIG-II) [ 83 , 84 ]; Traumatic Stress Symptoms: The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) [ 85 , 86 ]; Quality of Death: The Quality of Dying and Death questionnaire (QODD) [ 87 ]; and, Depressive Symptoms: Patient Health Questionnaire-9 (PHQ-9) [ 59 ].
Chart Review Form: Patients’ medical records will be reviewed at baseline and at each follow-up in order to document: i) medical diagnosis, date of diagnosis, and current cancer stage; ii) medical history including current comorbid medical and psychiatric diagnoses; iii) treatments received, including the timing of psychosocial oncology and/or palliative care interventions; and iv) emergent DD/suicidality events. We will obtain from the MAID clinical database the reasons of the patient and/or assessor-rated reasons for MAiD requests, MAiD approvals, MAiD completions, and non-completions.
Qualitative Interview: A semi-structured interview will be used. This interview guide will be further developed and reviewed as the constant comparative analysis progresses [ 90 ]; emerging themes in earlier interviews will serve to refine interview questions and probes. Open-ended enquiry will be made in the initial interview to understand the illness experience, including; caregiver stress, burden, support needs and support received, emotional and physical distress; attitudes about MAiD and advance directives. All interviews will be audiotaped, transcribed verbatim, verified and de-identified prior to analysis.
Data collection procedures
Baseline assessment.
Participants will be given the option of taking the questionnaire package home and returning the completed package in a self-addressed stamped envelope or completing it online. Participants will also be provided the option of having the questions read to them by a member of the research team as some participants may require this assistance due to their state of health. Medical data will be extracted from review of the medical record of each patient.
Longitudinal follow-up assessments
Participants will complete follow-up questionnaires every six months until study completion, unless they voluntarily withdraw, are unable to participate due to impairment in cognitive or physical functioning or die. An additional assessment will be made at the time of a MAiD request. Following the assessment, the medical record review will be updated. Where applicable, the date of death will be obtained from the medical record. In the case of patient death, participating primary caregivers will be followed-up approximately six months after this event to complete a bereavement assessment.
Qualitative assessments
Qualitative interviews will be conducted in a subset of the study participants. A quota sampling method [ 51 ] will be used to select a subset of patients and primary caregivers for one or more qualitative interview(s), conducted at six monthly intervals. Purposeful sampling will be based on high and low outcomes on the Schedule of Attitudes towards Hastened Death-Abbreviated (SAHD-A) (for patients) [ 58 ], caregiving burden and distress measures (for caregivers), and sociodemographic representation (for both patients and caregivers). We estimate that the saturation point will be reached at 10–15 participants per group, but we will recruit participants until saturation is reached. A grounded theory approach with constant-comparative analysis [ 90 ] will be used to identify themes and to determine the sample size at saturation point [ 91 ]. The interviews will last up to 60 min, depending upon the participants’ ability to participate, and will be conducted by a trained interviewer at the convenience of the participants over the telephone, in the clinic, or using a UHN-approved online platform. A frequency of six-monthly intervals was chosen in order to minimize participant burden but still capture as much of their longitudinal experience as possible. Enquiry will be made in follow-up interviews about issues raised in the first interview. Should a participating patient request MAiD, they, and their primary caregiver (if applicable), will be invited to complete an interview at that time, even if it falls between scheduled time points. Should a participating patient die during the study, either from MAiD or other causes, their primary caregiver (if applicable) will also be invited to complete one final semi-structured interview approximately six months after the patient’s death.
Data analysis
Survey data.
Descriptive statistics, desegregated by sex and gender, will be calculated to provide summary information about the characteristics of the participants at baseline. For each assessment time, descriptive statistics will be calculated for the DD outcomes and all other predictive variables. Prevalence of the DD, as measured by the SAHD-A, will be compared to our historical dataset [ 92 ]. The distributions of the continuous variables will be examined for non-normality, and transformations will be employed where necessary. Bivariate associations between DD variables and baseline medical and sociodemographic factors, as well as associations of these baseline variables with physical, psychosocial, and psychological risk factors will be described by calculating subgroup means and standard deviations for categorical variables and correlation coefficients for continuous variables.
The analysis of the longitudinal data will be conducted using mixed linear models (MLM), [ 93 ] which can take into account incomplete data and both time-varying and time-invariant predictors. To accommodate anticipated variations in individual profiles, random effects models will be fitted. MLM logistic regression will be used to determine predictors of both MAiD requests and completions. Similar exploratory analyses will be conducted to identify associations with emergent suicidality. We will replicate the MLM analysis from our previous study of the DD, [ 8 ] now incorporating receipt (or not) of psychosocial and/or palliative care interventions, and death anxiety as additional predictors of the DD (Fig. 1 ). To examine the statistical significance of interactions among medical, sociodemographic, physical, and psychosocial factors as suggested by the exploratory analyses, relevant interaction terms will be included in the MLMs. To avoid over-fitting the model, only those interactions regarded as clinically relevant will be tested in the model.
Qualitative interviews
A grounded theory approach will guide the qualitative data collection and analysis [ 94 ]. Conceptual categories and themes for coding will be derived directly from analyzing the interview material, with a view to inspecting deviant or negative cases in order to refine emerging propositions or hypotheses. This iterative process will continue until theoretical saturation is reached. The data analysis will use an inductive, constant comparison method to code or index the data. Once all data that matches that theme have been located, the process will be repeated to identify further themes or categories. Categories will be added to reflect the nuances in the data as possible. Cross-indexing will allow for the analysis of data items that fit into more than one category. Systematic comparative analysis will be used to identify differences and similarities between men and women, and those with and without a high DD (for patients), and with and without high caregiving burden and/or distress (for caregivers). Categories will also be examined in a longitudinal manner to identify patterns of emergence and development of categories over time and these finding will be compared to the quantitative data, particularly for the impact of goals of care conversations on desire for MAiD. Our analysis will be informed by our previous qualitative study on the DD [ 12 ].
Methodological strengths
This project is a longitudinal study of the course, predictors, and nature of the desire for MAiD in patients with advanced cancer in a geographic setting where MAiD is legally available. It includes quantitative and qualitative methods and uses a comprehensive battery of validated scales to measure the physical and psychosocial variables that we hypothesize are associated with the DD and MAiD requests and completions. The large study sample of patients and caregivers is a strength of the study design, enabling the evaluation of hypotheses in sub-groups. The study also will collect a wide range of sociodemographic information, which will enable the evaluation of the social determinants of the DD and MAiD, as well as examination of health equity in the receipt of MAiD. The quality of the research data collected will be ensured by having experienced, trained research personnel follow best research practices and institutional guidelines, including the use of standardized source notes and documentation of study participation in the patient’s clinical research record, to ensure rigour in the data collection processes. Research personnel will employ direct online data entry whenever possible; duplicate data entry for questionnaires completed in hard copy; and verification of transcribed interviews and all data extracted through medical chart review (e.g., disease and treatment-related data, supportive care services data, MAiD clinical data). Processes for confidentiality and secure storage of data have been ensured through REB approval, and data will be retained for 10 years post study completion as per REB guidelines at our institution. Further, all studies at PM are subject to internal audit by the Cancer Clinical Research Unit and/or the UHN Research Quality Integration teams, both of whom are independent of the study team.
Foreseeable limitations and mitigation strategies
The main challenge of this study is the requirement to recruit a large sample of patients with advanced or metastatic cancer and their primary caregivers. However, in our previous research experience with this population, we found that a 60% recruitment rate is achievable, without adverse effects from completion of a battery of measures of this kind [ 8 ]. Although there are a relatively large number of measures, we have minimized participant burden by limiting the number of measures administered longitudinally, selecting measures that are relatively brief or have been shortened from their original versions, offering the option of printed copy and online questionnaire completion at the hospital or at home, providing assistance with completion of questionnaires as requested in-person, online, or over the telephone, and conducting the qualitative interviews at the participants’ convenience. Participants with significant suicidality, physical or emotional distress identified by the research staff will be offered referral for psychosocial oncology and palliative care services in the Department of Supportive Care at PM, with notification to the attending oncologist with the patient’s consent. For caregivers (including bereaved caregivers) who express significant distress when completing the measures or qualitative interviews, a referral to the Department of Supportive Care’s Caregiver Clinic at PM for bereavement and/or psychosocial support will be offered.
Knowledge translation
Integral to the goals of this study is knowledge translation in the form of training healthcare providers to respond appropriately to expressions of the DD from patients in this new era of MAiD. Our findings will be directly incorporated into UHN MAiD training workshops, invited speaker engagements and the UHN MAiD website, to inform MAiD teams. Dissemination will occur through publications and conference presentations locally, nationally, and internationally, and as well as via the website of the Global Institute of Psychosocial, Palliative and End-of-Life Care (GIPPEC; see www.gippec.org ) and the Canadian Association of MAiD Assessors and Providers (CAMAP; see camapcanada.ca), thus bridging the knowledge to action gap.
Study implications
Data from this study will contribute significantly to our understanding of the DD in a setting where MAiD is legal, and inform critical questions regarding the utility of advance directives for MAiD, the management of depression in MAiD assessment, and how to guide healthcare providers in responding to DD statements with advanced cancer patients. The findings from this study will inform the training of oncologists and other healthcare providers in conversations about the DD and MAiD, and the assessment for MAiD eligibility through identifying distinctions between the DD, depressive suicidality, and the desire for MAiD in patients with advanced cancer. The results will also provide an evidence base to inform proposed changes in MAiD legislation, including the potential permissibility of MAiD in mental illness and as an advance directive.
Availability of data and materials
The datasets to be generated and/or analysed during the current study will not be publicly available due to institutional privacy and confidentiality guidelines. Additional information may be available from the corresponding authors on reasonable request.
The percentage of total cancer-related deaths in Canada was calculated by dividing MAID-related cancer deaths in 2020 (5,248) [ 4 ] by total cancer deaths in 2020 (83,300) [ 7 ].
Abbreviations
Caregiver Reaction Assessment scale
Death and Dying Distress Scale
Desire for Death
Desire for Hastened Death
Demoralization Scale-II
Diagnostic and Statistical Manual for Mental Disorders, 5th Edition
Duke University Religion Index
modified Experiences in Close Relationships scale
ENRICH Marital Satisfaction Scale (ENRICH)
Edmonton Symptom Assessment System-Revised (including constipation and sleep disturbances)
Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being scale
Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being-Non-Illness version
Modified FAMCARE Scale for Patients
Karnofsky Performance Status index
Medical Assistance in Dying
Mixed Linear Models
modified Medical Outcomes Study - Social Support Survey
Patient-Centered Communication-Cancer-6 items
Posttraumatic Stress Disorder Checklist for DSM-5
Patient Health Questionnaire-9
Princess Margaret Cancer Centre
Quality of Dying and Death questionnaire
Quality of Life at the End of Life – Cancer scale
Schedule of Attitudes towards Hastened Death-Abbreviated
short Orientation-Memory-Concentration Test
Self-Perceived Burden Scale
Texas Revised Inventory of Grief – Part II
University Health Network
Wish to Hasten Death
Will to Live Scale.
Carter v. Canada (Attorney General). Supreme Court Judgments 2015 SCC5. [Available from: https://scc-csc.lexum.com/scc-csc/scc-csc/en/item/14637/index.do . Accessed 16 July 2021.
Statutes of Canada. Chapter 3. An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying) Canada2016. [Available from: https://laws-lois.justice.gc.ca/eng/annualstatutes/2016_3/fulltext.html . Accessed 16 July 2021.
Bill C-7: An Act to amend the Criminal Code (medical assistance in dying). 2020. [Available from: https://www.justice.gc.ca/eng/csj-sjc/pl/charter-charte/c7.html ]. Accessed 16 July 2021.
Health Canada. Second Annual Report on Medical Assistance in Dying in Canada: 2020. Ottawa, ON; June 2021. [Available from: https://www.canada.ca/content/dam/hc-sc/documents/services/medical-assistance-dying/annual-report-2020/annual-report-2020-eng.pdf ]. Accessed 16 July 2021.
Health Canada. Fourth interim report on medical assistance in dying in Canada. In: Health Canada, editor. Ottawa: Health Canada; 2019. p. 1–12.
Rodin G, Shapiro GK, Wales J, Li M. Assisted dying in Canada: lessons from the first 3 years. In: Board RE, Bennet MI, Lewis P, Wagstaff J, Selby P, editors. End of life choices for cancer patients an international perspective. Oxford: EBN Health; 2020. p. 41–9.
Google Scholar
Canadian Cancer Society. Snapshot of incidence, mortality aand survival estimates by cancer type. Toronto: Canadian Cancer Society; 2020. [Available from: https://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics%20supplementary%20information/2020/2020_cancer-specific-stats.pdf?la=en ]. Accessed 16 July 2021.
Rodin G, Zimmermann C, Rydall A, Jones J, Shepherd FA, Moore M, et al. The desire for hastened death in patients with metastatic cancer. J Pain Symptom Manag. 2007;33(6):661–75. https://doi.org/10.1016/j.jpainsymman.2006.09.034 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Balaguer A. The wish to hasten death: a review of clinical studies. Psychooncology. 2011;20(8):795–804. https://doi.org/10.1002/pon.1839 .
Article PubMed Google Scholar
Balaguer A, Monforte-Royo C, Porta-Sales J, Alonso-Babarro A, Altisent R, Aradilla-Herrero A, et al. An international consensus definition of the wish to hasten death and its related factors. PLoS One. 2016;11(1):e0146184. https://doi.org/10.1371/journal.pone.0146184 .
Latha KS, Bhat SM. Suicidal behaviour among terminally ill cancer patients in India. Indian J Psychiatry. 2005;47(2):79–83. https://doi.org/10.4103/0019-5545.55950 .
Article CAS PubMed PubMed Central Google Scholar
Nissim R, Gagliese L, Rodin G. The desire for hastened death in individuals with advanced cancer: a longitudinal qualitative study. Soc Sci Med. 2009;69(2):165–71. https://doi.org/10.1016/j.socscimed.2009.04.021 .
Wilson KG, Dalgleish TL, Chochinov HM, Chary S, Gagnon PR, Macmillan K, et al. Mental disorders and the desire for death in patients receiving palliative care for cancer. BMJ Support Palliat Care. 2016;6(2):170–7. https://doi.org/10.1136/bmjspcare-2013-000604 .
Chochinov H, Wilson K, Enns M, Mowchun N, Lander S, Levitt M, et al. Desire for death in the terminally ill. Am J Psychiatry. 1995;152(8):1185–91. https://doi.org/10.1176/ajp.152.8.1185 .
Mystakidou K, Parpa E, Katsouda E, Galanos A, Vlahos L. The role of physical and psychological symptoms in desire for death: a study of terminally. Psychooncology. 2006;15(4):355–60. https://doi.org/10.1002/pon.972 .
Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity in the terminally ill: a cross-sectional, cohort study. Lancet. 2002;360(9350):2026–30. https://doi.org/10.1016/S0140-6736(02)12022-8 .
Kremeike K, Galushko M, Frerich G, Romotzky V, Hamacher S, Rodin G, et al. The DEsire to DIe in palliative care: optimization of management (DEDIPOM) - a study protocol. BMC Palliat Care. 2018;17(1):30. https://doi.org/10.1186/s12904-018-0279-3 .
Freeman S, Smith TF, Neufeld E, Fisher K, Ebihara S. The wish to die among palliative home care clients in Ontario, Canada: a cross-sectional study. BMC Palliat Care. 2016;15:24.
Article PubMed PubMed Central Google Scholar
Güell E, Ramos A, Zertuche T, Pascual A. Verbalized desire for death or euthanasia in advanced cancer patients receiving palliative care. Palliat Support Care. 2015;13(2):295–303. https://doi.org/10.1017/S1478951514000121 .
Hendry M, Pasterfield D, Lewis R, Carter B, Hodgson D, Wilkinson C. Why do we want the right to die? A systematic review of the international literature on the views of patients, carers and the public on assisted dying. Palliat Med. 2013;27(1):13–26. https://doi.org/10.1177/0269216312463623 .
Pacheco J, Hershberger PJ, Markert RJ, Kumar G. A longitudinal study of attitudes toward physician-assisted suicide and euthanasia among patients with noncurable malignancy. Am J Hosp Palliat Care. 2003;20(2):99–104. https://doi.org/10.1177/104990910302000207 .
Levene I, Parker M. Prevalence of depression in granted and refused requests for euthanasia and assisted suicide: a systematic review. J Med Ethics. 2011;37(4):205–11. https://doi.org/10.1136/jme.2010.039057 .
Hudson PL, Kristjanson LJ, Ashby M, Kelly B, Schofield P, Hudson R, et al. Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: a systematic review. Palliat Med. 2006;20(7):693–701. https://doi.org/10.1177/0269216306071799 .
Johansen S, Hølen JC, Kaasa S, Loge JH, Materstvedt LJ. Attitudes towards, and wishes for, euthanasia in advanced cancer patients at a palliative medicine unit. Palliat Med. 2005;19(6):454–60. https://doi.org/10.1191/0269216305pm1048oa .
Rosenfeld B, Pessin H, Marziliano A, Jacobson C, Sorger B, Abbey J, et al. Does desire for hastened death change in terminally ill cancer patients? Soc Sci Med. 2014;111:35–40. https://doi.org/10.1016/j.socscimed.2014.03.027 .
Emanuel EJ, Fairclough DL, Emanuel LL. Attitudes and desires related to euthanasia and physician-assisted suicide among terminally ill patients and their caregivers. JAMA. 2000;284(19):2460–8. https://doi.org/10.1001/jama.284.19.2460 .
Article CAS PubMed Google Scholar
Ohnsorge K, Gudat H, Rehmann-Sutter C. What a wish to die can mean: reasons, meanings and functions of wishes to die, reported from 30 qualitative case studies of terminally ill cancer patients in palliative care. BMC Palliat Care. 2014;13(1):38. https://doi.org/10.1186/1472-684X-13-38 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Mahtani-Chugani V, Balaguer A. What lies behind the wish to hasten death? A systematic review and meta-ethnography from the perspective of patients. PLoS One. 2012;7(5):e37117. https://doi.org/10.1371/journal.pone.0037117 .
Filiberti A, Ripamonti C, Totis A, Ventafridda V, De Conno F, Contiero P, et al. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. J Pain Symptom Manag. 2001;22(1):544–53. https://doi.org/10.1016/S0885-3924(01)00295-0 .
Article CAS Google Scholar
Smith KA, Harvath TA, Goy ER, Ganzini L. Predictors of pursuit of physician-assisted death. J Pain Symptom Manag. 2015;49(3):555–61. https://doi.org/10.1016/j.jpainsymman.2014.06.010 .
Article Google Scholar
Rosenfeld B, Breitbart W, Stein K, Funesti-Esch J, Kaim M, Krivo S, et al. Measuring desire for death among patients with HIV/AIDS: the schedule of attitudes toward hastened death. Am J Psychiatry. 1999;156(1):94–100. https://doi.org/10.1176/ajp.156.1.94 .
Rodin G, Lo C, Mikulincer M, Donner A, Gagliese L, Zimmermann C. Pathways to distress: the multiple determinants of depression, hopelessness, and the desire for hastened death in metastatic cancer patients. Soc Sci Med. 2009;68(3):562–9. https://doi.org/10.1016/j.socscimed.2008.10.037 .
Rodin G, Lo C, Rydall A, Shnall J, Malfitano C, Chiu A, et al. Managing Cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol. 2018;36(23):2422–32. https://doi.org/10.1200/JCO.2017.77.1097 .
Tan A, Zimmermann C, Rodin G. Interpersonal processes in palliative care: an attachment perspective on the patient-clinician relationship. Palliat Med. 2005;19(2):143–50. https://doi.org/10.1191/0269216305pm994oa .
Lo C, Lin J, Gagliese L, Zimmermann C, Mikulincer M, Rodin G. Age and depression in patients with metastatic cancer: the protective effects of attachment security and spiritual well-being. Ageing Soc. 2010;30(2):325–36. https://doi.org/10.1017/S0144686X09990201 .
Hillen MA, de Haes HC, Stalpers LJ, Klinkenbijl JH, Eddes EH, Verdam MG, et al. How attachment style and locus of control influence patients' trust in their oncologist. J Psychosom Res. 2014;76(3):221–6. https://doi.org/10.1016/j.jpsychores.2013.11.014 .
Oldham RL, Dobscha SK, Goy ER, Ganzini L. Attachment styles of Oregonians who request physician-assisted death. Palliat Support Care. 2011;9(2):123–8. https://doi.org/10.1017/S1478951510000660 .
Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada, and Europe. JAMA. 2016;316(1):79–90. https://doi.org/10.1001/jama.2016.8499 .
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol. 2017;3(10):1403–6. https://doi.org/10.1001/jamaoncol.2017.0243 .
Danyliv A, O’Neill C. Attitudes towards legalising physician provided euthanasia in Britain: the role of religion over time. Soc Sci Med. 2015;128:52–6. https://doi.org/10.1016/j.socscimed.2014.12.030 .
Moulton BE, Hill TD, Burdette A. Religion and trends in euthanasia attitudes among U.S. adults, 1977–2004. Sociol Forum. 2006;21(2):249–72. https://doi.org/10.1007/s11206-006-9015-5 .
Li M, Watt S, Escaf M, Gardam M, Heesters A, O'Leary G, et al. Medical assistance in dying - implementing a hospital-based program in Canada. N Engl J Med. 2017;376(21):2082–8. https://doi.org/10.1056/NEJMms1700606 .
Downar J, Fowler RA, Halko R, Huyer LD, Hill AD, Gibson JL. Early experience with medical assistance in dying in Ontario, Canada: a cohort study. CMAJ. 2020;192(8):E173–E81. https://doi.org/10.1503/cmaj.200016 .
Gamondi C, Fusi-Schmidhauser T, Oriani A, Payne S, Preston N. Family members' experiences of assisted dying: a systematic literature review with thematic synthesis. Palliat Med. 2019;33(8):1091–105. https://doi.org/10.1177/0269216319857630 .
Hales BM, Bean S, Isenberg-Grzeda E, Ford B, Selby D. Improving the medical assistance in dying (MAID) process: a qualitative study of family caregiver perspectives. Palliat Support Care. 2019;17(5):590–5. https://doi.org/10.1017/S147895151900004X .
Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. The hidden morbidity in cancer: spouse caregivers. J Clin Oncol. 2007;25(30):4829–34. https://doi.org/10.1200/JCO.2006.10.0909 .
Girgis A, Lambert SD, McElduff P, Bonevski B, Lecathelinais C, Boyes A, et al. Some things change, some things stay the same: a longitudinal analysis of cancer caregivers' unmet supportive care needs. Psychooncology. 2013;22(7):1557–64. https://doi.org/10.1002/pon.3166 .
Sklenarova H, Krümpelmann A, Haun MW, Friederich HC, Huber J, Thomas M, et al. When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer. 2015;121(9):1513–9. https://doi.org/10.1002/cncr.29223 .
Wang T, Molassiotis A, Chung BP, Tan JY. Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat Care. 2018;17(1):96. https://doi.org/10.1186/s12904-018-0346-9 .
Goldberg R, Nissim R, An E, Hales S. Impact of medical assistance in dying (MAiD) on family caregivers. BMJ Support Palliat Care. 2021;11(1):107-14. https://doi.org/10.1136/bmjspcare-2018-001686 .
Norman G, Streiner D. Biostatistics: The bare essentials. 3rd Edition. Shelton, Connecticut: People's Medical Publishing House; 2008.
Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–9. https://doi.org/10.1176/ajp.140.6.734 .
Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, editor. Evaluation of chemotherapeutic agents. New York: Columbia University Press; 1949. p. 191–205.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984;2(3):187–93. https://doi.org/10.1200/JCO.1984.2.3.187 .
Lo C, Burman D, Swami N, Gagliese L, Rodin G, Zimmermann C. Validation of the QUAL-EC for assessing quality of life in patients with advanced cancer. Eur J Cancer. 2011;47(4):554–60. https://doi.org/10.1016/j.ejca.2010.10.027 .
Grünke B, Philipp R, Vehling S, Scheffold K, Härter M, Oechsle K. Ea. measuring the psychosocial dimensions of quality of life in patients with advanced cancer: psychometrics of the German quality of life at the end of life-Cancer-psychosocial questionnaire. J Pain Symptom Manag. 2018;55(3):985–91. https://doi.org/10.1016/j.jpainsymman.2017.11.006 .
Carmel S. The will-to-live scale: development, validation, and significance for elderly people. Aging Ment Health. 2017;21(3):289–96. https://doi.org/10.1080/13607863.2015.1081149 .
Kolva E, Rosenfeld B, Liu Y, Pessin H, Breitbart W. Using item response theory (IRT) to reduce patient burden when assessing desire for hastened death. Psychol Assess. 2017;29(3):349–53. https://doi.org/10.1037/pas0000343 .
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Watanabe SM, Nekolaichuk C, Beaumont C, Johnson L, Myers J, Strasser F. A multi-Centre comparison of two numerical versions of the Edmonton symptom assessment system in palliative care patients. J Pain Symptom Manag. 2011;41(2):456–68. https://doi.org/10.1016/j.jpainsymman.2010.04.020 .
Hannon B, Dyck M, Pope A, Swami N, Banerjee S, Mak E, et al. Modified Edmonton symptom assessment system including constipation and sleep: validation in outpatients with cancer. J Pain Symptom Manag. 2015;49(5):945–52. https://doi.org/10.1016/j.jpainsymman.2014.10.013 .
Hui D, Bruera E. The Edmonton symptom assessment system 25 years later: past, present and future developments. J Pain Symptom Manag. 2017;53(3):630–43. https://doi.org/10.1016/j.jpainsymman.2016.10.370 .
Lo C, Burman D, Rodin G, Zimmerman C. Measuring patient satisfaction in oncology palliative care: psychometric properties of the FAMCARE-patient scale. Qual Life Res. 2009;18(6):747–52. https://doi.org/10.1007/s11136-009-9494-y .
Rosenberg M. Society and the adolescent self-image. Middletown: Wesleyan University Press; 1989.
Lo C, Hales S, Zimmermann C, Gagliese L, Rydall A, Rodin G. Measuring death-related anxiety in advanced cancer: preliminary psychometrics of the death and dying distress scale. J Pediatr Hematol Oncol. 2011;33(Supplement 2):S140–5. https://doi.org/10.1097/MPH.0b013e318230e1fd .
Krause S, Rydall A, Hales S, Rodin G, Lo C. Initial validation of the death and dying distress scale for the assessment of death anxiety in patients with advanced cancer. J Pain Symptom Manag. 2015;49(1):126–34. https://doi.org/10.1016/j.jpainsymman.2014.04.012 .
Shapiro GK, Mah K, Li M, Zimmerman C, Hales S, Rodin G. Validation of the Death and Dying Distress Scale in Patients with Advanced Cancer Psychooncology. 2020.
Reeve BB, Thissen DM, Bann CM, Mack N, Treiman K, Sanoff HK, et al. Psychometric evaluation and design of patient-centered communication measures for cancer care settings. Patient Educ Couns. 2017;100(7):1322–8. https://doi.org/10.1016/j.pec.2017.02.011 .
Kristjanson L. Validation and reliability testing of the FAMCARE scale: measuring family satisfaction with advanced cancer care. Soc Sci Med. 1993;36(5):693–701. https://doi.org/10.1016/0277-9536(93)90066-D .
Robinson S, Kissane DW, Brooker J, Hempton C, Michael N, Fischer J, et al. Refinement and revalidation of the demoralization scale: the DS-II - external validity. Cancer. 2016;122(14):2260–7. https://doi.org/10.1002/cncr.30012 .
Simmons LA. Self-perceived burden in cancer patients: validation of the self-perceived burden scale. Cancer Nurs. 2007;30(5):405–11. https://doi.org/10.1097/01.NCC.0000290816.37442.af .
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of Cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9. https://doi.org/10.1200/JCO.1993.11.3.570 .
Salsman JM, Garcia SF, Yanez B, Sanford SD, Snyder MA, Victorson D. Physical, emotional, and social health differences between posttreatment young adults with cancer and matched healthy controls. Cancer. 2014;120(15):2247–54. https://doi.org/10.1002/cncr.28739 . Accessed 16 July 2021.
Fowers BJ, Olson DH. ENRICH marital satisfaction scale: a brief research and clinical tool. J Fam Psychol. 1993;7(2):176–85. https://doi.org/10.1037/0893-3200.7.2.176 .
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. https://doi.org/10.1016/0277-9536(91)90150-B .
Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–16. https://doi.org/10.1016/j.jclinepi.2012.04.007 .
Koenig HG, Büssing A. The Duke University religion index (DUREL): a five-item measure for use in epidemiological studies. Religions. 2010;1(1):78–85. https://doi.org/10.3390/rel1010078 .
Kunce LJ, Shaver PR. An attachment-theoretical approach to caregiving in romantic relationships. In: Bartholomew K, Perlman D, editors. Attachment processes in adulthood, vol 5. Advances in personal relationships. London: Jessica Kingsley Publishers; 1994. p. 205–37.
Robinson S, Kissane DW, Brooker J, Michael N, Fischer J, Franco M, et al. Refinement and revalidation of the demoralization scale: the DS-II - internal validty. Cancer. 2016;122(14):2251–9. https://doi.org/10.1002/cncr.30015 .
Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15(4):271–83. https://doi.org/10.1002/nur.4770150406 .
Li M, Macedo A, Crawford S, Bagha S, Leung YW, Zimmermann C, et al. Easier said than done: keys to successful implementation of the distress assessment and response tool (DART) program. J Oncol Pract. 2016;12(5):e513–26. https://doi.org/10.1200/JOP.2015.010066 .
McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63. https://doi.org/10.1097/00005650-199303000-00006 .
Faschingbaur T, Zisook S, DeVaul R. The Texas revised inventory of grief. In: Zisook S, editor. Biopsychosocial aspects of bereavement. Washington: American Psychiatric Press, Inc.; 1987. p. 109–24.
Ringdal GI, Jordhoy MS, Ringdal K, Kaasa S. Factors affecting grief reactions in close family members to individuals who have died of cancer. J Pain Symptom Manag. 2001;22(6):1016–26. https://doi.org/10.1016/S0885-3924(01)00363-3 .
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–98. https://doi.org/10.1002/jts.22059 .
Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL- 5) in veterans. Psychol Assess. 2016;28(11):1379–91. https://doi.org/10.1037/pas0000254 .
Patrick DL, Engelberg RA, Curtis JR. Evaluating the quality of dying and death. J Pain Symptom Manag. 2001;22(3):717–26. https://doi.org/10.1016/S0885-3924(01)00333-5 .
Hales S, Zimmermann C, Rodin G. The quality of dying and death: a systematic review of measures. Palliat Med. 2010;24(2):127–44. https://doi.org/10.1177/0269216309351783 .
Lo C, Walsh A, Mikulincer M, Gagliese L, Zimmermann C, Rodin G. Measuring attachment security in patients with advanced cancer: psychometric properties of a modified and brief experiences in close relationships scale. Psychooncology. 2009;18(5):490–9. https://doi.org/10.1002/pon.1417 .
Strauss A, Corbin J. Basics of qualitative research. London: Sage; 1990.
Patton M. Qualitative evaluation and research methods. Newbury Park: Sage; 1990.
Lo C, Zimmermann C, Rydall A, Walsh A, Jones JM, Moore MJ, et al. Longitudinal study of depressive symptoms in patients with metastatic gastrointestinal and lung cancer. J Clin Oncol. 2010;28(18):3084–9. https://doi.org/10.1200/JCO.2009.26.9712 .
Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer; 2000.
Rennie D, Nissim R. The grounded theory method and humanistic psychology. In: Schneider K, Pierson J, Bugental J, editors. The handbook of humanistic psychology: leading edges in theory, practice, and research. 2nd ed. Thousand Oaks: Sage; 2015. p. 297–308.
Download references
Acknowledgements
We would like to thank Cassandra Graham for her input on the grant submission.
This study is funded by a competitive, peer-reviewed project grant awarded to ML and GR, co-principal investigators, from the Canadian Institutes of Health Research, Canada’s federal funding agency for health research (Grant No: CIHR PJT 401506; https://cihr-irsc.gc.ca ). An earlier version of our manuscript protocol underwent peer review by the funding body. GKS is supported by the Edith Kirchmann Postdoctoral Fellowship at PM, and by a CIHR 2019 Fellowship Award (CIHR MFE 171271). The funders of the study played no role in the study design, data collection, data analysis, data interpretation, or writing of this report.
Author information
Madeline Li and Gilla K. Shapiro are co-first authors.
Authors and Affiliations
Department of Supportive Care, Princess Margaret Cancer Centre, University Health Network, 620 University Avenue, 12th Floor, Toronto, Ontario, M5G 2C1, Canada
Madeline Li, Gilla K. Shapiro, Roberta Klein, Anne Barbeau, Anne Rydall, Jennifer A. H. Bell, Rinat Nissim, Sarah Hales, Camilla Zimmermann, Rebecca K. S. Wong & Gary Rodin
Department of Psychiatry, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada
Madeline Li, Jennifer A. H. Bell, Rinat Nissim, Sarah Hales, Camilla Zimmermann & Gary Rodin
Global Institute of Psychosocial, Palliative and End-of-Life Care (GIPPEC), University of Toronto and Princess Margaret Cancer Centre, Toronto, Ontario, Canada
Gilla K. Shapiro, Sarah Hales, Camilla Zimmermann & Gary Rodin
Joint Centre for Bioethics, University of Toronto, Toronto, Ontario, Canada
Jennifer A. H. Bell
Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Camilla Zimmermann
Department of Radiation Oncology, University of Toronto, Toronto, Ontario, Canada
Rebecca K. S. Wong
You can also search for this author in PubMed Google Scholar
Contributions
ML and GKS are co-first authors of this work. ML, GKS, AB, RK, AR, and GR made substantial contributions to the study design and writing of the manuscript. ML, GKS, RK, AB, AR, JAHB, RN, SH, CZ, RKSW and GR substantively revised the manuscript, read and approved the final submitted version, and guarantee the integrity of this work.
Corresponding authors
Correspondence to Madeline Li or Gilla K. Shapiro .
Ethics declarations
Ethics approval and consent to participate.
This study was approved on September 2, 2020 by the University Health Network Research Ethics Board (UHN REB #18–6182). All participants will provide written informed consent. Data collection is expected to begin by January 2021.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, M., Shapiro, G.K., Klein, R. et al. Medical Assistance in Dying in patients with advanced cancer and their caregivers: a mixed methods longitudinal study protocol. BMC Palliat Care 20 , 117 (2021). https://doi.org/10.1186/s12904-021-00793-4
Download citation
Received : 26 November 2020
Accepted : 09 June 2021
Published : 21 July 2021
DOI : https://doi.org/10.1186/s12904-021-00793-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Desire for hastened death
- Medical assistance in dying
- Medical communication
- Palliative care
- Assisted dying
- Will to live
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Medical Assistance in Dying: Patients', Families', and Health Care Providers' Perspectives on Access and Care Delivery
Affiliations.
- 1 Health Sciences Graduate Program, College of Medicine, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
- 2 Faculty of Nursing, University of Regina, Regina, Saskatchewan, Canada.
- 3 Department of Respirology, Critical Care, and Sleep Medicine, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
- 4 College of Medicine, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
- 5 Department of Community Health and Epidemiology, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
- 6 Department of Psychiatry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
- 7 Department of Anesthesiology, Perioperative Medicine and Pain Management, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
- 8 Provincial MAID Program, Saskatoon, Saskatchewan, Canada.
- PMID: 32302505
- DOI: 10.1089/jpm.2019.0509
Background: Medical assistance in dying (MAID) became legal in Canada in 2016. Although the legislation is federal, each province is responsible for establishing quality care. Objective: To explore patient, family, and health care provider (HCP) perspectives on MAID access and care delivery and improve regional MAID care delivery. Design: Qualitative exploratory. Setting/Subjects: We interviewed 5 patients (4 met the legislated MAID criteria and 1 did not), 11 family members (4 spouses, 5 children, 1 sibling, and 1 friend), and 14 HCP (3 physicians, 4 social workers, and 7 nurses) from June to August 2017. Measurement: Semistructured interviews, content analysis, and thematic summary. Results: Patients, families, and HCPs highlighted access and delivery concerns regarding program sustainability, care pathway ambiguity, lack of support for care choices, institutional conscientious objection (CO), navigating care in institutions with a CO, and postdeath documentation. Patients and families expressed additional concerns regarding lack of ability to provide advanced MAID consent, and the requirement of independent witnesses on MAID request forms and consent immediately before MAID administration. HCPs were additionally uncertain about professional roles and responsibilities. Ten recommendations to improve regional MAID care and the resultant practice change are presented. Conclusion: Quality improvement (QI) processes are essential to devise an accessible dignified patient- and family-centered MAID program. Ensuring patient and family perspectives are integrated into QI initiatives will assist programs in ensuring the needs of all are considered in structuring and staffing a program that is accessible, easy to navigate, and provides dignified end-of-life care in supportive and respectful work environments.
Keywords: access, quality improvement; medical assistance in dying; patient centered care; physician aid in dying.
PubMed Disclaimer
Similar articles
- Health care providers' ethical perspectives on waiver of final consent for Medical Assistance in Dying (MAiD): a qualitative study. Variath C, Peter E, Cranley L, Godkin D. Variath C, et al. BMC Med Ethics. 2022 Jan 30;23(1):8. doi: 10.1186/s12910-022-00745-4. BMC Med Ethics. 2022. PMID: 35094703 Free PMC article.
- How We Can Improve the Quality of Care for Patients Requesting Medical Assistance in Dying: A Qualitative Study of Health Care Providers. Oczkowski SJW, Crawshaw D, Austin P, Versluis D, Kalles-Chan G, Kekewich M, Curran D, Miller PQ, Kelly M, Wiebe E, Dees M, Frolic A. Oczkowski SJW, et al. J Pain Symptom Manage. 2021 Mar;61(3):513-521.e8. doi: 10.1016/j.jpainsymman.2020.08.018. Epub 2020 Aug 21. J Pain Symptom Manage. 2021. PMID: 32835830
- Implementation of Medical Assistance in Dying: A Scoping Review of Health Care Providers' Perspectives. Fujioka JK, Mirza RM, McDonald PL, Klinger CA. Fujioka JK, et al. J Pain Symptom Manage. 2018 Jun;55(6):1564-1576.e9. doi: 10.1016/j.jpainsymman.2018.02.011. Epub 2018 Feb 23. J Pain Symptom Manage. 2018. PMID: 29477968 Review.
- Access Isn't Enough: Evaluating the Quality of a Hospital Medical Assistance in Dying Program. Frolic A, Swinton M, Oliphant A, Murray L, Miller P. Frolic A, et al. HEC Forum. 2022 Dec;34(4):429-455. doi: 10.1007/s10730-022-09486-8. Epub 2022 Aug 26. HEC Forum. 2022. PMID: 36018528 Free PMC article.
- Professional experiences of formal healthcare providers in the provision of medical assistance in dying (MAiD): A scoping review. Ward V, Freeman S, Callander T, Xiong B. Ward V, et al. Palliat Support Care. 2021 Dec;19(6):744-758. doi: 10.1017/S1478951521000146. Palliat Support Care. 2021. PMID: 33781368 Review.
- Perspectives of Canadian health leaders on the relationship between medical assistance in dying and palliative and end-of-life care services: a qualitative study. Shapiro GK, Tong E, Nissim R, Zimmermann C, Allin S, Gibson JL, Lau SCL, Li M, Rodin G. Shapiro GK, et al. CMAJ. 2024 Feb 25;196(7):E222-E234. doi: 10.1503/cmaj.231241. CMAJ. 2024. PMID: 38408784 Free PMC article.
- A qualitative study of experiences of institutional objection to medical assistance in dying in Canada: ongoing challenges and catalysts for change. Close E, Jeanneret R, Downie J, Willmott L, White BP. Close E, et al. BMC Med Ethics. 2023 Sep 21;24(1):71. doi: 10.1186/s12910-023-00950-9. BMC Med Ethics. 2023. PMID: 37735387 Free PMC article.
- Barriers to connecting with the voluntary assisted dying system in Victoria, Australia: A qualitative mixed method study. White BP, Jeanneret R, Willmott L. White BP, et al. Health Expect. 2023 Dec;26(6):2695-2708. doi: 10.1111/hex.13867. Epub 2023 Sep 11. Health Expect. 2023. PMID: 37694553 Free PMC article.
- Institutional Resistance to Medical Assistance in Dying in Canada: Arguments and Realities Emerging in the Public Domain. Knox M, Wagg A. Knox M, et al. Healthcare (Basel). 2023 Aug 15;11(16):2305. doi: 10.3390/healthcare11162305. Healthcare (Basel). 2023. PMID: 37628502 Free PMC article.
- Canadian family members' experiences with guilt, judgment and secrecy during medical assistance in dying: a qualitative descriptive study. Crumley ET, LeBlanc J, Henderson B, Jackson-Tarlton CS, Leck E. Crumley ET, et al. CMAJ Open. 2023 Aug 22;11(4):E782-E789. doi: 10.9778/cmajo.20220140. Print 2023 Jul-Aug. CMAJ Open. 2023. PMID: 37607750 Free PMC article.
- Search in MeSH
LinkOut - more resources
Full text sources, miscellaneous.
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 24 October 2023
Medical assistance in dying for people living with mental disorders: a qualitative thematic review
- Caroline Favron-Godbout 1 &
- Eric Racine 1
BMC Medical Ethics volume 24 , Article number: 86 ( 2023 ) Cite this article
9056 Accesses
2 Citations
2 Altmetric
Metrics details
Medical assistance in dying (MAiD) sparks debate in several countries, some of which allow or plan to allow MAiD where a mental disorder is the sole underlying medical condition (MAiD-MD). Since MAiD-MD is becoming permissible in a growing number of jurisdictions, there is a need to better understand the moral concerns related to this option. Gaining a better understanding of the moral concerns at stake is a first step towards identifying ways of addressing them so that MAiD-MD can be successfully introduced and implemented, where legislations allow it.
Thus, this article aims (1) to better understand the moral concerns regarding MAiD-MD, and (2) to identify potential solutions to promote stakeholders’ well-being. A qualitative thematic review was undertaken, which used systematic keyword-driven search and thematic analysis of content. Seventy-four publications met the inclusion criteria.
Various moral concerns and proposed solutions were identified and are related to how MAiD-MD is introduced in 5 contexts: (1) Societal context , (2) Healthcare system , (3) Continuum of care , (4) Discussions on the option of MAiD-MD , (5) MAiD-MD practices . We propose this classification of the identified moral concerns because it helps to better understand the various facets of discomfort experienced with MAiD-MD. In so doing, it also directs the various actions to be taken to alleviate these discomforts and promote the well-being of stakeholders.
The assessment of MAiD-MD applications, which is part of the context of MAiD-MD practices, emerges as the most widespread source of concern. Addressing the moral concerns arising in the five contexts identified could help ease concerns regarding the assessment of MAiD-MD.
Peer Review reports
Medical assistance in dying (MAiD), which encompasses euthanasia and physician-assisted suicide [ 1 ], raises debate in several countries. Belgium, The Netherlands, Luxembourg, and Switzerland have allowed people living with mental disorders to access some forms of MAiD for years [ 2 ]. More recently, Spain has passed a MAiD law making people living with mental disorders eligible for MAiD under certain conditions [ 3 ]. Canada has decriminalized MAiD for physical conditions and plans to allow MAiD when a mental disorder is the sole underlying medical condition (MAiD-MD) [ 4 ]. The subject of MAiD-MD is a delicate and controversial one, which has given rise to a great deal of international reflection, leading to the development of a rich literature on the subject. Hence, the literature on MAiD-MD is extensive, and research emerging from countries that allow this practice is complemented by contributions from countries that do not. An important part of the reflections and work carried out on the subject regards the question of whether people living with mental disorders should be eligible for MAiD or not. Literature reviews on the arguments in favor and against MAiD-MD have notably been carried out by Nicolini et al. (2020) and Grassi et al. (2022) [ 5 , 6 ]. The ethical acceptability of MAiD-MD practices is a polarizing issue, which can limit the exploration of nuances in positions and impede the mutual understanding of people with different perspectives on this question. We believe that a promising notion for exploring these nuances is that of moral concerns, as they may provide common ground for discussion between those in favor and those against MAiD-MD. Indeed, moral concerns may be part of the reasons why some people are opposed to MAiD-MD, but also of the drawbacks that those in favor of MAiD-MD feel are important to address if the practice is to be acceptable. For example, moral concerns about the conciliation of MAiD-MD practices and suicide prevention practices may lead some people to oppose MAiD-MD, just as it may qualify the position of those in favor of MAiD-MD (e.g., being in favor on condition that requests for MAiD-MD are not the result of suicidal impulses).
Considering that MAiD-MD is becoming permissible in a growing number of jurisdictions, there is a need to better understand the moral concerns related to this practice. Gaining this understanding is a first step towards identifying ways of addressing them so that MAiD-MD can be successfully introduced and implemented, where legislations allow it. Thus, this article aims (1) to better understand the moral concerns regarding MAiD-MD, and (2) to highlight potential solutions that have been suggested by others to promote stakeholders’ well-being (namely people living with mental disorders, their relatives, and their healthcare professionals). Hence, although highly relevant, moral concerns relating to not allowing MAiD for people with psychiatric suffering are not covered by this literature review.
This qualitative thematic review relied on systematic literature searches in addition to screening and structured thematic content extraction strategy, inspired by Arksey & O’Malley (2005) and by Levac & al. (2010), as well as by more structured forms of thematic literature reviews [ 7 , 8 , 9 , 10 , 11 , 12 ]. Figure 1 illustrates the article selection process in the form of a PRISMA-type diagram.
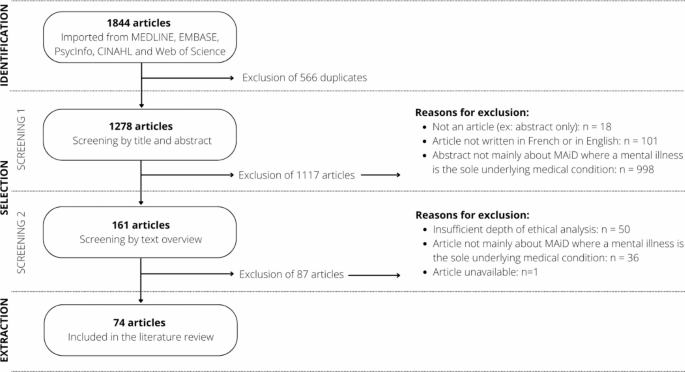
PRISMA diagram illustrating the systematic article selection process
Identifying the research question: The following questions guided the review: What moral concerns are reported regarding medical assistance in dying where a mental disorder is the sole underlying medical condition? What possible solutions are proposed to address these concerns?
Identifying relevant studies: The literature searches were developed around three concepts: moral concerns, medical assistance in dying, and mental disorders. The search strategy was validated by a librarian from Université de Montréal’s School of Public Health and put forward MeSH terms (Medical Subject Headings) and keywords for each concept, which were applied to the title, abstract, and keyword headings fields. Moral concerns were identified using the “ethics” and “morals” MeSH terms, with the equation (Moral* or bioethic* or ethic*); medical assistance in dying was targeted using the MeSH terms “suicide, assisted”, and “euthanasia, active, voluntary”, with the equation ((Assist* or “medical aid”) ADJ2 (dying or dead or death or suicide or die)) or euthanas*; mental disorders were targeted with the “mental disorders” MeSH term, with the equation mental disorder* or mental health or mental illness* or psychiatric disorder* or psychiatric illness* or psychiatric disease* or behavior disorder* or bipolar* or depress* or psychos* or psychot* or schizoaffect* or schizphren* or cyclothym* or anxiety* or obsessive-compulsive disorder* or post-traumatic stress* or dissociat* disorder* or personality disorder* or eating disorder* or social phobia or substance-related disorder*. The literature search was conducted on July 13, 2022, in the MEDLINE (n = 641), EMBASE (n = 509), CINAHL (n = 170), PsycInfo (n = 268) and Web of Science (n = 256) databases, and the identified articles were imported into the Covidence software (N = 1278).
Study selection: Article selection was conducted in two phases: (1) by the title and the abstract, (2) by the content overview. The inclusion criteria for the first screening phase were: that it is an article and not a poster or conference abstract; that the article is written in French or in English (languages mastered by the authors); that the abstract of the article focuses on MAiD-MD. This first screening phase allowed for 161 articles to move to the second screening phase. Articles were excluded if MAiD-MD was not central to the abstract; if they dealt with MAiD in a context other than mental disorders (e.g., MAiD only, MAiD for physical conditions or for life fatigue, MAiD in the context of neurocognitive or neurodevelopmental disorders, MAiD for minors and newborns); if they dealt with suicide only or palliative care; if they dealt with involuntary euthanasia (e.g., Nazi era); or if they addressed moral concerns unrelated to MAiD-MD (e.g., veterinary euthanasia, health ethics in general). The inclusion criteria for the second phase were: that the article focuses on MAiD-MD (e.g., an article about MAiD but with more than minimal content about MAiD-MD); that the article offers substantial qualitative analysis either by their methods (qualitative design) or by qualitatively appraising quantitative data (quantitative design); that the article mentions moral concerns related to MAiD-MD (e.g., an article about the eligibility criteria for MAiD-MD and discussing related moral concerns). This second screening phase allowed for the inclusion of 74 articles. Articles were excluded if MAiD-MD was a minor portion of the article (e.g., if only a brief paragraph alluded to MAiD-MD); if the qualitative contribution of the article was limited or absent (e.g., survey results presented with little interpretative analysis); or if the content was purely clinical. Inclusion criteria were piloted and established by the first author and a research assistant, who independently reviewed each article, and were validated by the second author. Disagreements were resolved through dialogue and contributed to the refinement of inclusion criteria.
Charting the data: The content extraction was carried out by the first author to identify moral concerns emerging from the literature as well as possible solutions to address them. A moral concern was identified when discomfort, distress, uncertainty, or a dilemma as to the best way to act was identified [ 13 ] or if a described situation impeded stakeholders’ well-being [ 14 ]. Articles were classified as (1) theoretical article; (2) perspective, opinion, response, or comment; (3) review; (4) empirical study; (5) case review or case series; (6) chapter.
Collating, summarizing, and reporting the results: A thematic analysis allowed us to identify moral concerns and to group them into five contexts of emergence, as illustrated in Additional file 1. We have also identified potential solutions proposed in the literature and associated them with the context of emergence to which they correspond. Narrative summaries citing illustrative studies are presented to highlight these moral concerns and proposed solutions. Salient constructs, which recur in several contexts, have been identified in the discussion.
Consultation: Following Levac et al. (2010)’s steps for realizing a scoping review, this literature review included a consultation phase with a group of key stakeholders, including people living with a mental disorder, to complement the literature review [ 11 , 12 ]. The group’s comments and experiential knowledge were considered to improve the formulation of some of the identified moral concerns and to shed better light on some of them.
The keyword-driven searches yielded 74 publications corresponding to the inclusion criteria, of which 18/74 came from jurisdictions currently allowing MAiD-MD (Belgium, The Netherlands, Switzerland), 22/74 came from a country planning to expand its legislation (Canada), 19/74 were from places where MAiD-MD is not considered (USA, Africa, Australia, other countries in Europe), and 14/74 were combined international perspectives. Among these publications, 29/74 were theoretical articles; 28/74 were comments or perspectives; 7/74 were reviews; 4/74 were empirical studies; 4/74 were case studies; and 2/74 were chapters.
This qualitative thematic review allowed us to identify various moral concerns and possible solutions, which are related to how MAiD-MD is introduced into the following 5 contexts of emergence: (1) societal context , (2) healthcare system , (3) continuum of care , (4) discussions on the option of MAiD-MD , (5) MAiD-MD practices . These contexts were identified iteratively during data extraction and are interrelated as shown in Fig. 2 .
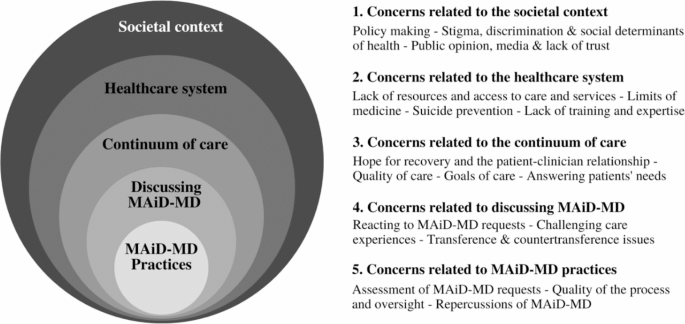
Five contexts of emergence of moral concerns related to MAiD-MD
Societal context
Moral concerns related to the societal context, policy making and tension between inclusion and protection.
In the societal context, the primary moral concern surrounding MAiD-MD relates to developing laws, policies, and regulations. On the one hand, the need to protect people living with mental disorders is highlighted, given their possible vulnerability [ 15 , 16 , 17 ]. On the other hand, excluding these people from eligibility for MAiD-MD is seen as an obstacle to their right to die with dignity [ 18 ]. Laws governing MAiD try to take this tension into account. However, concerns remain about the societal responsibility to help these people live with their condition before considering helping them to die [ 18 , 19 ]. Although MAiD-MD can bring some peace of mind [ 18 , 20 , 21 ] by offering an exit option to people who fear that their suffering will be perpetual [ 22 ], concerns have been expressed about the message sent by the expansion of MAiD eligibility to potentially vulnerable people [ 23 ], who may be struggling to find meaning to their lives [ 24 ]. The fear that the gradual expansion of the laws governing MAiD could lead to abuses is also noted [ 25 , 26 ].
Stigma, discrimination, and social determinants of health
The introduction of MAiD-MD raises fears of increased stigmatization and discrimination about mental disorders and the fear that problems related to social determinants of health may lead some people to consider seeking MAiD-MD. Discrimination can be experienced by people with mental disorders on a daily basis, both by the people around them [ 27 ], by the authorities [ 28 ], by the medical profession [ 17 ], or by public policies that exclude them or fail to consider them adequately [ 16 , 29 , 30 , 31 , 32 ]. Experiences of stigma have been reported as contributing more to the intolerability of suffering among people with mental disorders than the symptoms of the disorder [ 33 ]. Some socially disadvantaged people might consider MAiD-MD to escape the suffering and stressors caused by their reality [ 6 ], such as social isolation, homelessness, poverty, inadequate housing, and unemployment [ 33 , 34 ]. Thus, people could ask for MAiD-MD to escape life circumstances that are in principle remediable (e.g., with policy and decisions regarding resource allocation [ 35 ]).
Public opinion, media and lack of trust
Some authors fear MAiD-MD may lead to or increase the erosion of patient and public trust in psychiatry [ 25 , 36 ] by reinforcing the belief that nothing can be done to help people living with mental disorders [ 37 ]. The growing media coverage of controversial examples of MAiD-MD can amplify this lack of trust [ 37 ] by opening a space of doubt and fear in the collective imagination [ 38 ] and by influencing policymaking. Finally, a history of mistreatment towards people with mental disorders generates a taboo around MAiD-MD [ 39 ].
Identified needs and proposed solutions to societal context issues
A critical need is to help people live with their mental disorders before considering helping them die, which requires improving social support [ 40 ], reducing stigma [ 41 ], adapting work environments to mental health needs, and fostering a sense of community belonging [ 42 ]. It is essential to examine the legislative developments surrounding MAiD-MD [ 43 ] to ensure that the suffering of people living with mental disorders is not minimized [ 44 ] and to promote their empowerment in their care decisions as well as in their life trajectories, which may or may not include a request for MAiD-MD [ 38 ].
Healthcare system
Moral concerns related to the healthcare system, lack of resources and access to care and services.
Human, financial, and material resource shortages [ 34 , 45 , 46 ] are acute in mental health care and services. In this context, adding a more rigorous assessment process for MAiD-MD requests, including various safeguards, could impose an additional burden on an already struggling system [ 28 , 45 ]. Furthermore, access to adequate and patient-centered mental health care is essential to alleviate suffering. However, many people living with mental disorders face significant delays in accessing care and services [ 46 ] or do not have access to treatments and services adapted to their condition at all [ 43 ]. MAiD-MD could thus be considered an alternative to care, which is deemed problematic [ 19 , 47 ]. Although this possibility may suggest that it is preferable not to allow MAiD-MD in a context where resources and access to resources are lacking, preventing people in unbearable suffering from accessing MAiD-MD on the pretext that the healthcare system must be improved beforehand is to condemn prima facie eligible people to excruciating suffering [ 34 ].
Limits of medicine
The fact that, despite decades of research, medicine remains an imprecise discipline that cannot answer every problem is difficult to accept for some healthcare professionals [ 48 ]. It can make them reluctant to conclude that a mental disorder is without prospect of recovery; hence, to consider a MAiD-MD request ineligible. In some cases, the lack of effectiveness of mental health treatments [ 49 ] can make healthcare professionals feel powerless or dread situations where they cannot help certain people [ 41 ]. Furthermore, when quality mental health care fails to help patients, they may be confined to intolerable suffering unless MAiD-MD is considered [ 48 ]. The fact that the causes of mental disorders are often misunderstood limits the chances that effective treatments adapted to the patient’s needs will be available [ 50 , 51 ].
Suicide prevention
The main concern surrounding MAiD-MD and suicide prevention is the idea that MAiD-MD is a way of helping some people commit suicide [ 49 , 52 ]. Therefore, MAiD-MD seems complicated to reconcile with suicide prevention [ 53 , 54 ], with suicide prevention being a well-established societal responsibility [ 47 ]. Some healthcare professionals perceive MAiD-MD as a way to act on suicidal ideation, resulting in the death of people who would not otherwise have committed this act [ 52 ]. Thus perceived, MAiD-MD runs counter to the commitment of healthcare professionals to preserve life by preventing suicide [ 47 ]. However, data from a recent empirical study reported that people living with mental disorders have no difficulty distinguishing their previous suicidal states from their state when they requested MAiD-MD [ 20 ]. This suggests that the reasons leading a person to seek MAiD-MD may differ significantly from those leading them to commit suicide.
Lack of training and expertise
A lack of training and expertise from healthcare professionals could impede the introduction of MAiD-MD in the healthcare system [ 55 , 56 ]. Some healthcare professionals feel ill-prepared to follow the law, failing to know how it applies to patients [ 56 ] and how to apply it without discrimination [ 33 ] (e.g., without being influenced by biases against mental disorders). Others feel a lack of preparation to receive MAiD-MD requests and to get involved in MAiD-MD [ 55 , 56 ], either due to a lack of communication skills [ 57 ], lack of knowledge of mental disorders [ 33 , 58 ] or lack of reflexivity and ethical deliberation skills [ 56 ].
Identified needs and proposed solutions to healthcare system issues
Among the proposed solutions, having better-resourced mental health services is necessary [ 16 , 40 ]. The need to show humility in the face of the limits of psychiatry in relieving mental suffering [ 24 ] is reported, and the need to improve access to mental health care and services is also expressed [ 34 , 42 , 45 , 57 ]. The importance of raising awareness of suicide risk and its management is mentioned too [ 37 ]. In addition, a glaring need is felt among healthcare professionals for training [ 42 , 56 ] and guidelines considering the complexity encountered in practice [ 59 ], and both healthcare professionals, MAiD-MD applicants, and their relatives would benefit from these resources being developed.
Continuum of care
Moral concerns related to the continuum of care, hope for recovery and the patient-clinician relationship.
The introduction of MAiD-MD into the continuum of care can affect the therapeutic relationship [ 17 , 48 , 59 ], which is closely correlated with patients’ hope for improvement [ 37 ], a key facilitator of recovery [ 23 , 52 ]. Healthcare professionals’ involvement or support of MAiD-MD could also affect the resilience of patients [ 60 ], the therapeutic relationship [ 26 , 48 , 60 ] and potentially influence the patient to lose hope that their situation will improve if they have the impression that the healthcare professional is abandoning the therapeutic project [ 23 , 37 ]. Such loss of hope can give rise to a self-fulfilling prophecy [ 23 , 37 , 51 ] by reinforcing the patient’s sense of hopelessness and compromising their potential for recovery [ 51 ]. Conversely, some authors point out that acknowledging the irremediability of a person’s condition can promote hope, empathy and engagement and thus promote recovery [ 33 ], making that person feel genuinely considered [ 37 ].
Quality of care
Another primary concern surrounds the quality and continuity of care [ 19 ], and adding MAiD-MD as an option exacerbates this concern [ 23 , 54 ]. The fear that MAiD-MD might hinder the improvement of care practices, social support, and resources to help people live with their mental disorders has been expressed [ 37 , 41 ]. It is problematic that a person could request MAiD-MD without first accessing care and services adapted to their situation [ 61 , 62 ]. For example, Mehlum et al. (2020) mentioned doubting whether people living with borderline personality disorder are offered evidence-based personality disorder-specific treatments. This suggests that people living with mental disorders may seek medical assistance in dying while not receiving the best treatments for their condition [ 63 ]. A Dutch empirical study reported that some people who requested MAiD-MD felt they were being refused some therapeutic options because their mental healthcare professional deemed treatment incompatible with a wish for MAiD-MD [ 20 ]. A lack of holistic care for people living with mental disorders has also been documented: psychosocial dimensions and interactional factors are often overlooked compared to biological dimensions [ 23 ]. Being regularly confronted with patients with suicidal ideation, healthcare professionals can involuntarily adopt paternalistic attitudes towards these people [ 64 ], which affects their quality of care.
Goals of care
MAiD-MD may seem irreconcilable with the valuing of recovery-oriented approaches in mental health care [ 65 ], and some fear that its introduction into the continuum of care will cause a paradigm shift from a goal of improving quality of life towards a goal of assessing eligibility for MAiD-MD [ 28 ]. Helping people live with their mental disorders should precede MAiD-MD [ 66 ]. Still, the goals of care should also be tailored to each person’s specific needs, preferences, and life goals, including the right to refuse treatments, and the need to recognize when interventions become futile [ 2 , 32 , 61 , 62 , 64 , 67 ]. Healthcare professionals may find themselves uncertain about how best to act in the face of treatment refusals, believing that these refusals can lead to preventable deaths [ 4 ] and considering that alleviating suffering through MAiD-MD takes time away from patients, limiting opportunities for healthcare professionals to provide significant therapeutic benefits [ 38 ]. Determining the futility of interventions is a difficult value judgment to make for both healthcare professionals and patients [ 32 , 64 ].

Answering patients’ needs
Among the unmet needs of people living with mental disorders are those related to care and services (notably a lack of symptom relief), but also those related to daily needs (notably the need to have satisfying relationships) and existential needs (especially the difficulty of finding meaning to life) [ 16 , 20 , 68 ]. The lack of response to these needs can prevent them from having a satisfactory quality of life [ 31 ]. This lack of help in living with mental disorders may lead some people to conclude that MAiD-MD is the only option susceptible to alleviate their suffering. Although MAiD-MD may be an option adapted to the needs of some people living with mental disorders, they must have prior access to options likely to help them live with their condition, knowing that they may decide not to choose these options. These options may include, but are not limited to, healthcare, social services, adapted housing and community support.
Identified needs and proposed solutions to continuum of care issues
Quality care involves adopting a non-paternalistic attitude towards people living with mental disorders [ 31 , 69 ]. Reasonable therapeutic alternatives should be tried before considering MAiD-MD [ 18 , 22 ] while considering the patient’s values. Thus, a change in psychotherapeutic or pharmacological strategy or a change in physician or care setting should first be considered before concluding that no options are left to help the person. For some, the mere possibility of having access to MAiD-MD could be enough to lighten the burden of their mental disorder without feeling the need to take advantage of it [ 20 , 21 ]. It is essential to cultivate the therapeutic relationship, to maintain open communication, and to offer support to address existential questions [ 70 ]. Recognizing and considering their moral convictions may help healthcare professionals be more mindful about discussing MAiD-MD with patients [ 28 ]. Communication should be patient-friendly, and the uncertainty related to mental disorders explicitly recognized [ 71 ], choosing words so as not to undermine hope (e.g., avoiding saying that nothing more can be done to help the person [ 72 ]). Some underline the attention that palliative psychiatry should receive when the mental disorder has reached a certain chronicity, as it could help alleviate some suffering of mental disorders [ 37 , 41 , 70 ]. These avenues seem promising for helping people living with mental disorders lead meaningful lives and maintain a positive view of themselves [ 62 ]. Two-track approaches to MAiD-MD, which maintain recovery-oriented care in parallel with the assessment of MAiD-MD requests, are also reportedly promising [ 40 , 69 ].
Discussions on the option of MAiD-MD
The context of discussions on the option of MAiD-MD refers to the period of reflection surrounding this option as well as the request itself. A person may consider requesting MAiD-MD and wish to talk about it with those around them and their clinicians, then decide to go ahead or not. Consideration of MAiD-MD may include a request for MAiD-MD, which will then be explored through discussions before moving on to assessment (which is part of the context of MAiD-MD practices).
Moral concerns related to discussing the option of MAiD-MD
Reacting to maid-md requests.
Since MAiD-MD is a morally sensitive practice with which not everyone agrees, it can be difficult for healthcare professionals to receive requests for MAiD-MD, to respond to them in a way that suits the patient’s needs, to involve the family or not, and to adapt the treatment goals. It can also be challenging for family members to accept that their loved one intends to request or has requested MAiD-MD [ 24 ]. Perception conflicts can arise between patients and healthcare professionals [ 71 , 73 ], whose training focuses mainly on preserving life, particularly when MAiD-MD is not considered a last resort because treatment options remain to be tried [ 22 ]. The way of receiving and responding to the request for MAiD-MD can be tinged with paternalism aimed at imposing healthcare professionals’ values on patients [ 48 ] or reveal a lack of empathy or sensitivity to their situation [ 39 ], which can increase the distress of applicants. A person who requests MAiD-MD and is simply told that they are not eligible or that they are not there yet may feel frustration [ 20 ], even distress. MAiD-MD requests place a significant emotional burden on the healthcare professionals who receive and assess them [ 24 , 55 ], particularly if they are conscientious objectors [ 45 ] or if these requests make them feel powerless to protect people with mental disorders [ 41 , 53 ]. Conscientious objectors can oppose MAiD-MD without ignoring the suffering at stake: assuming the opposite is a mistake [ 74 ]. The experience of being overburdened by the number or the weight of the requests also leads some healthcare professionals to refrain from participating in MAiD [ 55 ]. Moreover, having a loved one die from MAiD-MD can be distressing for relatives [ 55 ], who may need to reconcile the hope that the patient will recover with the support they want to provide [ 6 ]. Although the involvement of relatives can be beneficial to better understand the situation of the person requesting MAiD-MD, confidentiality issues also arise when it comes to whether or not to involve relatives in the discussions surrounding MAiD-MD [ 45 , 75 ].
Challenging care experiences influencing discussions
Many people with mental disorders have difficult care experiences. These people are sometimes met without compassion or even with exasperation, which can affect their self-esteem and increase their marginalization [ 19 ]. Mental suffering can be difficult to understand [ 24 , 48 ] and tends to be less recognized than the suffering arising from physical illnesses [ 15 , 21 , 39 ]. People living with mental disorders are often not taken seriously [ 20 , 48 ] unless they have physical symptoms or somatic manifestations. Even that is not always enough to make them be taken seriously. They may then feel helpless, which may lead them to seek MAiD-MD. This request can be well considered [ 42 ], but it can also be a cry for help in order to be seen and heard [ 20 , 70 ], or a request for communication [ 63 ]. The moral, cultural, or professional biases of healthcare professionals can alter the quality of the care experience [ 37 ]. Thus, biases against psychiatric distress can lead healthcare professionals to conclude that the person’s suffering is exaggerated and only in their head [ 32 ].
Transference and countertransference issues
MAiD-MD can generate issues of transference and countertransference, in particular given the enduring relationship that some patients have with their healthcare professional [ 2 , 28 , 53 , 59 , 60 , 71 , 76 ]. A healthcare professional could involuntarily be overinvested [ 41 ] or identify too much with the patient’s situation [ 2 , 46 ] and show them an excess of empathy because they fear the state of deterioration, suffering, and loneliness experienced by the patient. This transposition of the healthcare professional’s emotions onto the situation would constitute countertransference. A healthcare professional could share the patient’s demoralization [ 57 ] from lack of being able to relieve their suffering [ 28 ]: this transposition of the patient’s despair onto the healthcare professional would constitute transference. Transference and countertransference often come together and are usually unconscious, but they can lead healthcare professionals to facilitate access to MAiD-MD, or to respond to a MAiD-MD request with hostility, which could subsequently make a patient reluctant to share their suicidal thoughts, push them to act on those suicidal thoughts, or lead them to change healthcare professionals, thus harming the continuity of care [ 28 ]. The ability to bear the suffering reported by patients while containing their feeling of helplessness is a major personal and relational challenge for healthcare professionals, who are often ill-prepared for this type of communication [ 57 ]. Identifying their own feelings of countertransference is also difficult for healthcare professionals [ 59 ], who may lack perspective of their situation.
Identified needs and proposed solutions related to discussing MAiD-MD
The fundamental recommendation concerning the management of MAiD-MD requests is related to the way of receiving and responding to them. Whether the applicant is eligible or not, requests for MAiD-MD should be welcomed with openness and empathy, and should be considered seriously [ 70 ]. These requests can be received first as a demand for human connection and professional expertise to relieve suffering [ 70 ], but they must also be considered as real requests for assistance in dying to which it is important to respond in a meaningful way [ 42 ]. Feeling that their suffering is acknowledged and having the opportunity to talk about their request for MAiD-MD can ease the suffering of people living with mental disorders, give them hope, build trust in the therapeutic relationship, and lead them to consider new therapeutic avenues, or decrease their desire to die [ 20 , 58 ]. This requires facilitating communication through deliberation and considering the important values of all stakeholders [ 65 , 70 ] as well as the needs of the MAiD-MD applicant. The issues of transference and countertransference should be addressed through professional consultations where the observations, feelings, and motivations of healthcare professionals would be shared with the consulted colleagues to gain better insight into possible situations of countertransference [ 71 ]. However, this might not always be sufficient [ 59 ].
MAiD-MD practices
Moral concerns related to maid-md practices and their repercussions, assessment of maid-md requests.
The assessment of requests is the dimension of MAiD-MD that has received the most attention in the literature. The underlying moral concerns are manifold and relate to the complexity of the assessment of MAiD-MD requests [ 56 , 58 ]; as well as to the interpretation and application of eligibility criteria [ 6 , 56 ], mainly in relation to capacity [ 29 , 77 , 78 ], to the intolerability of suffering [ 17 , 56 , 64 , 70 ], and to the irremediability of the condition [ 47 , 51 ]. The vagueness of the concepts of incurability and irremediability, as well as the complexity of assessing the applicant’s level of appreciation of their situation, have also been highlighted [ 45 , 55 , 77 , 79 ]. With respect to capacity to consent, many authors are concerned that requests for MAiD-MD can be influenced by the mental disorder and that the desire to die can be a symptom of the disorder, or that the request for MAiD-MD can stem from external pressure [ 6 , 41 , 45 ], which would invalidate the voluntary nature of the request [ 56 , 80 ]. When remediable external factors are driving the request, the concern that MAiD-MD could become a permanent solution to a temporary problem is palpable [ 22 , 81 ].
Cognitive distortions resulting from the disorder could invalidate the informed nature of the requests [ 47 ], but this is not always the case [ 44 , 79 ]. The lack of stability of the desire to die, understood as a lack of continuity in the desire to obtain MAiD-MD, emerges as a concern [ 2 ]. The fluctuating nature of capacity also complicates its assessment [ 27 , 48 ]. The question of the intolerability of suffering highlights the subjective nature of this assessment by both the applicant and the healthcare professional [ 44 , 58 ]. Knowing that the perceived acceptability of an intervention varies across patients [ 27 ], it can be difficult for healthcare professionals to confirm that a person’s suffering is intolerable [ 46 ]. Attempting to objectively assess suffering can also lead to insensitivity towards a person’s unique experiences of states they consider intolerable [ 49 ]. In terms of the irremediability of the condition, the diagnostic and prognostic uncertainty complicates the assessment of eligibility for MAiD-MD [ 82 ], in particular because the possibility that a future intervention will succeed in alleviating the suffering still exists [ 38 ], but also because refusing treatment can add a layer of complexity to the assessment of irremediability [ 5 ]. Rooney et al. (2018) point out, however, that it is epistemically impossible to know with certainty that a person will never recover, and that to require such certainty in assessment condemns some people to suffer without considering the reality of their experiences [ 16 ].
Quality of the process and oversight
The interpretive leeway enjoyed by healthcare professionals complicates the task of ensuring the quality, rigor and consistency of the MAiD-MD request assessment process [ 2 , 19 , 28 , 37 ]. The concern that some healthcare professionals could feel pressured to acquiesce to a request for MAiD-MD because it seems the least harmful avenue for a patient demonstrating chronic suicidality is also implied [ 22 ]. In addition, the subjectivity of the assessment increases the risk that it – or the discussions it relies on – contains biases, particularly in relation to the clinical experience, beliefs and values of healthcare professionals [ 28 ], or because of existing prejudices against mental disorders (e.g., assuming that all people living with mental disorders lack decision making capacity) [ 32 , 43 , 61 ]. Although collaborative work and discussions between healthcare professionals can limit the impact of biases on the assessment process [ 71 ], some assessing healthcare professionals seem reluctant to involve other healthcare professionals who do not bear decision-making responsibility (e.g., members of the healthcare team who know the patient well) [ 56 ]. The length and complexity of the assessment process makes some healthcare professionals uncomfortable about having to refuse a request for MAiD-MD [ 55 ], or even leads them not to get involved in this practice [ 46 ]. Concerns about appropriate safeguards have been raised, including the lack of referral to a psychiatrist [ 37 ]; the use of a third party that can impose an arbitrarily high capacity threshold while neglecting the context behind the MAiD-MD request [ 48 ]; or the imposition of a longer minimum period between the request and MAiD-MD implementation [ 48 ]. Freeland et al. (2022) point out that where some believe that the nature of mental disorders warrants additional safeguards, others consider the imposition of specific measures to be discriminatory [ 45 ]. Questions are also raised regarding the quality of regulatory oversight processes for MAiD-MD [ 37 , 75 ] and the best type of oversight process to implement retrospectively or prospectively [ 45 ].
Repercussions of MAiD-MD
Concerns related to the repercussions of MAiD-MD include the risk of error in the assessment of requests, the burden and moral distress that can accompany this practice, as well as the possibility that the patients feel left to fend for themselves or are pushed towards suicide. Errors in assessment could result in some patients being incorrectly deemed eligible, and vice versa [ 19 , 47 ]. They could also put healthcare professionals at risk of sanctions, and some point to a need to protect healthcare professionals in this sense [ 56 ]. The burden of bearing the decision can be heavy for healthcare professionals [ 6 ]. Some of them may experience moral distress if they think the eligibility criteria for MAiD-MD do not take into consideration key features of certain mental disorders, like fluctuating suicidal ideations and behaviours [ 6 ]. One article deplored that some healthcare professionals believe that patients who have the physical capacity to commit suicide should do so rather than resort to MAiD-MD and to the resources this practice mobilizes [ 31 , 48 ]. Several authors express a profound unease with this idea, knowing that letting the patient take matters into their own hands can lead to a violent and isolated death or to an even more painful situation in the event of a failed suicide attempt [ 30 , 41 , 63 ]. In this sense, Berghmans et al. (2013) express that people living with mental disorders generally do not have the means to end their life with dignity without the help of healthcare professionals [ 71 ]. An alternative to MAiD-MD could be voluntarily stopping eating and drinking, but MAiD-MD is perceived as being more humane [ 30 , 68 ]. The fate of patients being refused MAiD-MD [ 83 ], as well as the impact of MAiD-MD on loved ones [ 55 ] and on other people living with mental disorders [ 59 , 68 ], are noted as morally concerning and remain understudied.
Identified needs and proposed solutions to issues with MAiD-MD practices
The literature is replete with questions to address in relation to MAiD-MD, including the feeling of being a burden [ 20 , 69 ]; safeguards to implement or avoid [ 30 , 56 , 69 ]; factors reducing the voluntariness of MAiD-MD requests [ 46 ]; the relevance of adopting a more holistic consideration of certain eligibility criteria, by better considering the quality of life and the needs of patients [ 48 ]; the importance of developing resources oriented towards aid in living, etc. A need for training [ 78 ], awareness-raising [ 27 ], and guidelines [ 78 ] is apparent, as well as a need to develop more support resources to help all stakeholders through the challenging situations and discussions that can arise in the context of MAiD-MD [ 64 , 70 , 84 ].
Critical analysis of the literature on MAiD-MD
The thematic analysis of available publications has made it possible to identify various moral concerns and possible remediations, which are related to how MAiD-MD is introduced in five contexts of emergence. The societal context can influence some people towards MAiD-MD because of stigmatizing experiences or difficult living conditions. The healthcare system poses certain barriers to living with a mental disorder, both through limited access to insufficient resources, as well as gaps in knowledge, medical training and suicide prevention. The continuum of care is challenged with respect to quality of care, response to needs, goals of care, hope and the therapeutic relationship. Those who wish to discuss the MAiD-MD option encounter relational and communication challenges. MAiD-MD practices are complicated by different types of uncertainty, both in the assessment of MAiD-MD applications and in the quality and repercussions of the processes. The assessment of MAiD-MD applications, which is part of the context of MAiD-MD practices, is the most recurrent source of concern but addressing the various moral concerns that emerge upstream of MAiD-MD (e.g., moral concerns emerging in the other four contexts identified) could indirectly facilitate the assessment of requests.
Three general observations emerge from this review. First, based on the sample of literature included in this review, we observe a lack of qualitative empirical studies reporting the perspectives of people living with mental disorders and their relatives. Second, we note points of convergence in the literature: certain morally concerning constructs transcend the contexts of emergence and thus seem particularly worrying. Third, taking a critical look at the possible solutions, we note that they are mainly oriented towards what should be done to remedy the concerns, without proposing how to do so.
Lack of qualitative empirical studies
Only 4 of the 74 articles included are qualitative empirical studies, and only one directly relates to the moral concerns of people living with mental disorders: the others deal with the perspectives of clinicians. The remaining 70 articles are contributions from clinicians or from academics. Among these articles, some (e.g., comments written by clinicians) relate the moral concerns of patients or relatives, but this is done indirectly, via the interpretation of the authors. Based on the consulted literature, the perspectives of patients and their relatives thus seem poorly documented, and their being often reported by others can influence how they are communicated. However, a growing body of empirical qualitative research on medical assistance in dying for people with mental disorders has emerged in recent years [ 85 , 86 , 87 ]. Some relevant articles, which would have emerged with a search strategy focusing solely on medical assistance in dying and mental disorders, may have been overlooked by the search strategy. It may be the case because when someone talks about their experience or shares their perspective on a sensitive subject, the moral dimensions of these experiences are not always made explicit, despite being implicitly present. Further enrichment of this body of empirical qualitative literature by clarifying the moral aspects of lived experience would increase our understanding of the discomfort experienced by those involved in medical assistance in dying for mental health reasons.
Points of convergence in the literature
The classification of moral concerns by contexts of emergence has enabled us to identify that four morally concerning constructs recur in different contexts. The fact that a given problem occurs in several ways, particularly in different contexts, suggests that it is widespread. We believe that the recurrence of these problematic constructs suggests the importance of addressing them as a priority. The first is stigma, experienced in society but also in care experiences. The second relates to the notion of burden: MAiD-MD entails a certain level of burden, particularly for the healthcare system; for clinicians feeling the weight of their professional responsibility in the context of care and MAiD-MD; for loved ones and clinicians feeling helpless in the face of persistent suffering. The third construct relates to relational and communication challenges arising in the care trajectory, upstream and downstream of requests for MAiD-MD: biases, uneasiness and judgments can show through in communication, and some people can then feel distress. The fourth construct concerns the factors influencing the request for MAiD-MD: environmental factors, other people and the mental disorder itself can alter the autonomous nature of the request by influencing it unduly. Although not all requests for MAiD-MD are marked by these influences, it is important to be attentive to them in order to prevent requests from being accepted when other options could have better met the needs of the applicants.
Critical look at moral concerns and proposed solutions
Given the large number of moral concerns documented, it is essential, on the one hand, to prioritize certain concerns that seem more important or more recurrent, as we have undertaken to do by identifying specific points of convergence in the literature. On the other hand, we need to consider the source of these moral concerns. Considering that moral concerns are lived by people and thus form part of their experience, we recognize that all moral concerns can be genuinely worrying for the people who experience them but that some may have to be addressed at source. For example, some moral concerns may stem from misunderstanding the laws or practices of medical assistance in dying. They emerge from a lack of information and can therefore be addressed more quickly than others, notably by explaining the laws, practices, and implications more clearly.
Moreover, in the current literature, the proposed solutions are generally oriented towards “what to do” to remedy a given moral concern – ideas for addressing the problems are proposed – without explaining “how” to remedy the problem in order to promote the well-being of those concerned. For example, if communication issues are interfering with the clinician-patient relationship, the importance of open communication will be emphasized, as will the importance of cultivating the therapeutic relationship, but the recommendations will generally not go as far as to suggest “how to do this”. However, while “how to” ideas are not well documented in the scientific literature, some in-depth reports emerging from the grey literature, notably in Canada, go further, accompanying their “what to do” recommendations with a few pointers to guide “how” this might be implemented locally. For a given moral concern, it would seem promising to develop, with the concerned stakeholders, tools or resources that are adapted to each emergence context. For example, stigma could be addressed at the societal level through awareness campains, and at the healthcare level through training tailored to the nuances and subtleties of stigma and self-stigma. While stigma is not specific to MAiD-MD, it can significantly affect how MAiD-MD requests are responded to and assessed and how people living with mental disorders experience the process. The prejudice that leads some people to consider anyone living with a mental disorder de facto unfit to make a legitimate request for medical assistance in dying can also lead to systematic refusals of those requests. Thus, different reversible factors that may unduly influence the request for MAiD-MD could be tackled before considering going forward with MAiD-MD. In order to limit difficult relational experiences, tools could be developed to improve the recognition of biases: this type of introspection exercise could help communication in care, as well as in the reception and assessment of MAiD-MD applications. Facilitating difficult discussions could also be beneficial in easing the burden felt by different stakeholders. Finally, although certain moral concerns relating to MAiD-MD seem particular to the context of mental disorders, several of them could emerge in the context of MAiD more broadly, and thus, the solutions to answer them may have already been developed in physical MAiD, and could therefore be applied in the context of mental disorders.
A first limitation of this review is the methodological choice of excluding the grey literature, which has inevitably led us not to consider relevant reflection work on MAiD-MD such as the recent Final Report of Canada’s Expert Panel on MAiD and Mental Illness [ 88 ]. A second limitation is that considering that the moral dimensions of human experience are often implicit, the methodological choice of limiting the literature search to writings containing keywords related to ethics or morality in addition to keywords related to MAiD and mental disorders may have excluded some relevant articles. A third limitation is that given the qualitative orientation of this review, the search was restricted to publications with a certain depth of qualitative analysis. Some relevant articles, such as quantitative empirical research, could thus have been discarded. A fourth limitation is that certain disorders, such as neurocognitive disorders, autism spectrum disorders and intellectual disabilities, were excluded for the sake of not grouping overly heterogeneous conditions together, but certain identified moral concerns identified in this review could still concern those groups. We excluded the articles on those disorders in order to delimitate clearly the literature review. Also, we consider that the potential similarities in the experienced moral concerns should be demonstrated, not assumed.
MAiD-MD raises fundamental ethical concerns that need to be addressed. This literature review is one of the first to look at the moral concerns related to MAiD-MD and possible solutions to address them. We hope that this advancement will guide the development of resources, interventions or support tools aimed at improving the experiences of people living with mental disorders, their loved ones and healthcare professionals, who experience these concerns.
Data Availability
Not applicable.
Abbreviations
Medical Assistance in Dying (in a context of) Mental Disorder
Medical Subject Headings
Deschamps P. Les soins de fin de vie: repères éthiques, juridiques et sociétaux. LexisNexis; 2017.
Calati R, Olie E, Dassa D, Gramaglia C, Guillaume S, Madeddu F, et al. Euthanasia and assisted suicide in psychiatric patients: a systematic review of the literature. J Psychiatr Res. 2021;135:153–73.
Google Scholar
Ramos-Pozón S, Terribas-Sala N, Falcó-Pegueroles A, Román-Maestre B. Persons with mental disorders and assisted dying practices in Spain: an overview. Int J Law Psychiatry. 2023;87:101871.
van Veen SMP, Evans N, Ruissen AM, Vandenberghe J, Beekman ATF, Widdershoven GAM. Irremediable psychiatric suffering in the context of medical assistance in dying: a delphi-study. Can J Psychiatry. 2022;67(10):758–67.
Nicolini ME, Kim SYH, Churchill ME, Gastmans C. Should euthanasia and assisted suicide for psychiatric disorders be permitted? A systematic review of reasons. Psychol Med. 2020;50(8):1241–56.
Grassi L, Folesani F, Marella M, Tiberto E, Riba MB, Bortolotti L, et al. Debating euthanasia and physician-assisted death in people with psychiatric disorders. Curr Psychiatry Rep. 2022;24(6):325–35.
Barned C, Rochette M, Racine E. Voluntary decision-making in addiction: a comprehensive review of existing measurement tools. Conscious Cogn. 2021;91:103115.
Bracken-Roche D, Bell E, Karpowicz L, Racine E. Disclosure, consent, and the exercise of patient autonomy in surgical innovation: a systematic content analysis of the conceptual literature. Acc Res. 2014;21(6):331–52.
Saigle V, Racine E. Ethical challenges faced by healthcare professionals who care for suicidal patients: a scoping review. Monash Bioeth Rev. 2018;35(1):50–79.
Saigle V, Seguin M, Racine E. Identifying gaps in suicide research: a scoping review of ethical challenges and proposed recommendations. IRB. 2017;39(1):1–9.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Quintal A, Hotte É, Racine E. Morality as experienced: a scoping review of moral matters encountered by adults living with rare diseases. Philos Ethics Humanit Med. (Under review).
Ryff CD, Singer BH. Know thyself and become what you are: a eudaimonic approach to psychological well-being. J Happiness Stud. 2008;9(1):13–39.
Tanner R. An ethical-legal analysis of medical assistance in dying for those with mental illness. Alta L Rev. 2018;56:149.
Rooney W, Schuklenk U, van de Vathorst S. Are concerns about irremediableness, vulnerability, or competence sufficient to justify excluding all psychiatric patients from medical aid in dying? Health Care Anal. 2018;26(4):326–43.
Reel K, Macri R, Dembo JS, Bean S, Shanker RR, Costa L, et al. Assisted death in mental health: our last, best judgement–assisted death for intolerable, irremediable suffering in mental health–substance use. Ethics in Mental Health-Substance Use: CRC Press; 2017. pp. 293–314.
Provencher-Renaud G, Larivée S, Sénéchal C. L’accès à l’aide médicale à mourir pour les personnes souffrant de troubles mentaux. Ann Med Psychol. 2019;177(8):801–8.
Yarascavitch A. Assisted dying for mental disorders: why Canada’s legal approach raises serious concerns. 2017. Available at SSRN 2988535.
Pronk R, Willems DL, van de Vathorst S. Feeling seen, being heard: perspectives of patients suffering from mental illness on the possibility of physician-assisted death in the Netherlands. Cult Med Psychiatry. 2022;46(2):475–89.
Wilson C. Psychiatry’s last taboo. New Sci. 2016;231(3083):16–7.
Cowley C. Euthanasia in psychiatry can never be justified. A reply to Wijsbek. Theor Med Bioeth. 2013;34(3):227–38.
Blikshavn T, Husum TL, Magelssen M. Four reasons why assisted dying should not be offered for depression. J Bioeth Inq. 2017;14(1):151–7.
Simpson AIF. Medical assistance in dying and mental health: a legal, ethical, and clinical analysis. Can J Psychiatry. 2018;63(2):80–4.
Jones RM, Simpson AI. Medical assistance in dying: challenges for psychiatry. Front Psychiatry. 2018;9:678.
Naudts K, Ducatelle C, Kovacs J, Laurens K, Van Den Eynde F, Van Heeringen C. Euthanasia: the role of the psychiatrist. Br J Psychiatry. 2006;188(5):405–9.
Shaffer CS, Cook AN, Connolly DA. A conceptual framework for thinking about physician-assisted death for persons with a mental disorder. Psychol Public Policy Law. 2016;22(2):141–57.
Benrimoh D, Perreault A, Van Den Eynde F. Euthanasia requests in a Canadian psychiatric emergency room: a case series: part 1 of the McGill University euthanasia in psychiatry case series. Int J Law Psychiatry. 2017;55:37–44.
Steinbock B. Physician-assisted death and severe, treatment-resistant depression. Hastings Cent Rep. 2017;47(5):30–42.
Schuklenk U, van de Vathorst S. Treatment-resistant major depressive disorder and assisted dying. J Med Ethics. 2015;41(8):577–83.
Dembo J, Schuklenk U, Reggler J. For their own good: a response to popular arguments against permitting medical assistance in dying (MAID) where mental Illness is the sole underlying condition. Can J Psychiatry. 2018;63(7):451–6.
Cholbi MJ. The terminal, the futile, and the psychiatrically disordered. Int J Law Psychiatry. 2013;36(5–6):498–505.
Gaind KS. What does irremediability in mental illness mean? Can J Psychiatry. 2020;65(9):604–6.
Downie J, Schuklenk U. Social determinants of health and slippery slopes in assisted dying debates: lessons from Canada. J Med Ethics. 2021;47(10):662–9.
Ho A, Norman JS. Social determinants of mental health and physician aid-in-dying: the real moral crisis. AJOB. 2019;19(10):52–4.
Buturovic Z. Embracing slippery slope on physician-assisted suicide and euthanasia could have significant unintended consequences. J Med Ethics. 2020.
Courtet P, Olié E. Legislation and ethics of physician-assisted suicide and euthanasia in psychiatric patients: evidence from Benelux. In: Wasserman D, Wasserman C, Wasserman D, editors. Oxford textbook of suicidology and suicide prevention. Oxford University Press; 2021.
Kirby J. Medical assistance in dying for suffering arising from mental health disorders: could augmented safeguards enhance its ethical acceptability? JEMH. 2016.
Hirsch J. The wish to die: assisted suicide and mental illness. J Soc Work End-of-Life Palliat Care. 2016;12(3):231–5.
Verhofstadt M, Van Assche K, Sterckx S, Audenaert K, Chambaere K. Psychiatric patients requesting euthanasia: guidelines for sound clinical and ethical decision making. Int J Law Psychiatry. 2019;64:150–61.
Dembo JS. Addressing treatment futility and assisted suicide in psychiatry. JEMH. 2010.
Macri R, Wagner F, Stuckey MI. A values-based analysis of recovery-oriented practice in mental health care and medical assistance in dying. Can J Commun Ment Health. 2020;39(2):1–10.
Biggs H, Diesfeld K. Assisted suicide for people with depression: an advocate’s perspective. Med Law Int. 1995;2(1):23–37.
Dembo J, van Veen S, Widdershoven G. The influence of cognitive distortions on decision-making capacity for physician aid in dying. Int J Law Psychiatry. 2020;72:101627.
Freeland A, Godkin D, Dembo J, Chan P, Knoops F, Lachmann M, et al. Medical assistance in dying (MAiD) for persons whose sole underlying medical condition is a mental disorder: challenges and considerations. Can J Psychiatry. 2022;67(1):71–87.
Pronk R, Evenblij K, Willems DL, van de Vathorst S. Considerations by Dutch psychiatrists regarding euthanasia and physician-assisted suicide in psychiatry: a qualitative study. JCP. 2019;80(6):14494.
Miller FG, Appelbaum PS. Physician-assisted death for psychiatric patients - misguided public policy. N Engl J Med. 2018;378(10):883–5.
Bahji A, Delva N. Making a case for the inclusion of refractory and severe mental Illness as a sole criterion for canadians requesting medical assistance in dying (MAiD): a review. J Med Ethics. 2022;48(11):929–34.
Kious BM, Battin M. Physician aid-in-dying and suicide prevention in psychiatry: a moral crisis? AJOB. 2019;19(10):29–39.
Żuradzki T, Nowak PG. Deep uncertainties in the criteria for physician aid-in-dying for psychiatric patients. AJOB. 2019;19(10):54–6.
Hatherley JJ. Is the exclusion of psychiatric patients from access to physician-assisted suicide discriminatory? J Med Ethics. 2019;45(12):817–20.
Mack RA, Stanton CE. Responding to terminal anorexia nervosa: three cases and proposed clinical characteristics. J Eat Disord. 2022;10(1):87.
Denys D. Is euthanasia psychiatric treatment? The struggle with death on request in the Netherlands. Am J Psychiatry. 2018;175(9):822–3.
Sinyor M, Schaffer A. The lack of adequate scientific evidence regarding physician-assisted death for people with psychiatric disorders is a danger to patients. Can J Psychiatry. 2020;65(9):607–9.
Deschepper R, Distelmans W, Bilsen J. Requests for euthanasia/physician-assisted suicide on the basis of mental suffering: vulnerable patients or vulnerable physicians? JAMA Psychiatry. 2014;71(6):617–8.
Demedts D, Roelands M, Libbrecht J, Bilsen J. The attitudes, role & knowledge of mental health nurses towards euthanasia because of unbearable mental suffering in Belgium: a pilot study. J Psychiatr Ment Health Nurs. 2018;25(7):400–10.
Kissane DW, Kelly BJ. Demoralisation, depression and desire for death: problems with the Dutch guidelines for euthanasia of the mentally ill. Aust N Z J Psychiatry. 2000;34(2):325–33.
Dom G, Stoop H, Haekens A, Sterckx S. Euthanasia and assisted suicide in the context of psychiatric disorders: sharing experiences from the low countries. Psychiatr Pol. 2020;54(4):661–72.
Schoevers RA, Asmus FP, Van Tilburg W. Physician-assisted suicide in psychiatry: developments in the Netherlands. Psychiatr Serv. 1998;49(11):1475–80.
Lemmens T. When a theoretical commitment to broad physician aid-in-dying faces the reality of its implementation. Am J Bioeth. 2019;19(10):65–8.
Trachsel M, Jox RJ. Suffering is not enough: assisted dying for people with mental illness. Bioethics. 2022;36(5):519–24.
Vandenberghe J. Physician-assisted suicide and psychiatric illness. N Engl J Med. 2018;378(10):885–7.
Mehlum L, Schmahl C, Berens A, Doering S, Hutsebaut J, Kaera A, et al. Euthanasia and assisted suicide in patients with personality disorders: a review of current practice and challenges. Borderline Personal Disord Emot Dysregul. 2020;7:15.
Pienaar W. Developing the language of futility in psychiatry with care. S Afr J Psychiatr. 2016;22(1):978.
Winkler L, Wetterauer C. Provide access to information on assisted suicide for a patient with a diagnosis of depression? An ethics consultation. GeroPsych. 2021;34(2):57–62.
Gevers JK. Physician-assisted suicide and the Dutch courts. Camb Q Healthc Ethics. 1996;5(1):93–9.
Zhong R, Xu Y, Oquendo MA, Sisti DA. Physician aid-in-dying for individuals with serious mental illness: clarifying decision-making capacity and psychiatric futility. Am J Bioeth. 2019;19(10):61–3.
Nicolini ME, Gastmans C, Kim SYH. Psychiatric euthanasia, suicide and the role of gender. Br J Psychiatry. 2022;220(1):10–3.
Stoll J, Ryan CJ, Trachsel M. Perceived burdensomeness and the wish for hastened death in persons with severe and persistent mental illness. Front Psychiatry. 2020;11:532817.
Liégeois A. Euthanasia and mental suffering: an ethical advice for Catholic mental health services. Christ Bioeth. 2013;19(1):72–81.
Berghmans R, Widdershoven G, Widdershoven-Heerding I. Physician-assisted suicide in psychiatry and loss of hope. Int J Law Psychiatry. 2013;36(5–6):436–43.
Hurwitz TA. Euthanasia in mental illness: a four part series: part II: sadness and suicidality: why mentally ill patients request euthanasia. JEMH. 2016.
Frati P, Gulino M, Mancarella P, Cecchi R, Ferracuti S. Assisted suicide in the care of mentally ill patients: the Lucio Magri’s case. J Forensic Leg Med. 2014;21:26–30.
Nicolini ME, Gastmans C, Kim SYH. Parity arguments for ‘physician aid-in-dying’ (PAD) for psychiatric disorders: their structure and limits. Am J Bioeth. 2019;19(10):3–7.
Pearce S. Invited commentary on … When unbearable suffering incites psychiatric patients to request euthanasia: a qualitative study. Br J Psychiatry. 2017;211(4):246–7.
Kirby J. Medical assistance in dying for suffering arising from mental health disorders: could augmented safeguards enhance its ethical acceptability? JEMH. 2017.
Broome MR, de Cates A. Choosing death in depression: a commentary on treatment-resistant major depressive disorder and assisted dying. J Med Ethics. 2015;41(8):586–7.
Sheehan K, Gaind KS, Downar J. Medical assistance in dying: special issues for patients with mental illness. Curr Opin Psychiatry. 2017;30(1):26–30.
Brodeur J, Links PS, Boursiquot PE, Snelgrove N. Medical assistance in dying for patients with borderline personality disorder: considerations and concerns. Can J Psychiatry. 2022;67(1):16–20.
Hall W, Parker M. The need to exercise caution in accepting addiction as a reason for performing euthanasia. Addiction. 2018;113(7):1178–80.
Olie E, Courtet P. The advocates of euthanasia in patients with mental illness are going in the wrong direction. Br J Psychiatry. 2019;214(3):171.
van Veen SMP, Scheurleer WFJ, Ruijsch ML, Röder CH, Widdershoven GAM, Batalla A. Last-minute recovery of a psychiatric patient requesting physician-assisted death. Psychiatr Serv. 2020;71(6):621–3.
Verhofstadt M, Audenaert K, Van Assche K, Sterckx S, Chambaere K. Ghent University Hospital’s protocol regarding the procedure concerning euthanasia and psychological suffering. BMC Med Ethics. 2019;20(1):59.
Verhofstadt M, Audenaert K, Mortier F, Deliens L, Liégeois A, Pardon K, et al. Concrete experiences and support needs regarding the euthanasia practice in adults with psychiatric conditions: a qualitative interview study among healthcare professionals and volunteers in Belgium. Front Psychiatry. 2022;13:859745.
Verhofstadt M, Pardon K, Audenaert K, Deliens L, Mortier F, Liégeois A, et al. Why adults with psychiatric conditions request euthanasia: a qualitative interview study of life experiences, motives and preventive factors. J Psychiatr Res. 2021;144:158–67.
Verhofstadt M, Chambaere K, Pardon K, Mortier F, Liégeois A, Deliens L, et al. The impact of the euthanasia assessment procedure: a qualitative interview study among adults with psychiatric conditions. BMC Psychiatry. 2022;22(1):435.
Verhofstadt M, Audenaert K, Van den Broeck K, Deliens L, Mortier F, Titeca K, et al. Euthanasia in adults with psychiatric conditions: a descriptive study of the experiences of Belgian psychiatrists. Sci Prog. 2021;104(3):368504211029775.
Gupta M, Carter RM. Final report of the expert panel on MAiD and mental illness. Ottawa, Ontario: Health Canada; 2022.
Download references
Acknowledgements
The authors would like to thank Élissa Hotte for help in the study selection and Grace Feeney for editorial assistance. The authors would also like to express their appreciation to the Pragmatic Health Ethics Research Unit team members and to Catherine Perron, Julie Lafond, Luc Vigneault, Simon Courtemanche and Jocelyne Saint-Arnaud who commented on a previous version of this manuscript.
The literature review, the stakeholder consultation and the writing of this manuscript are supported by a grant from the Réseau québécois sur le suicide, les troubles de l’humeur et les troubles associés (ER), a doctoral grant from the Fonds de recherche du Québec – Santé (2021–2025) (CFG), and a career award from the Fonds de recherche du Québec – Santé (ER).
Author information
Authors and affiliations.
Pragmatic Health Ethics Research Unit, Montreal Clinical Research Institute, 110 av. des Pins O, Montreal, QC, H2W 1R7, Canada
Caroline Favron-Godbout & Eric Racine
You can also search for this author in PubMed Google Scholar
Contributions
Both authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by CFG. The first draft of the manuscript was written by CFG and ER commented on previous versions of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Eric Racine .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Favron-Godbout, C., Racine, E. Medical assistance in dying for people living with mental disorders: a qualitative thematic review. BMC Med Ethics 24 , 86 (2023). https://doi.org/10.1186/s12910-023-00971-4
Download citation
Received : 23 April 2023
Accepted : 15 October 2023
Published : 24 October 2023
DOI : https://doi.org/10.1186/s12910-023-00971-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying
- Physician assisted Suicide
- Mental disorders
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
- DOI: 10.1136/bmjspcare-2018-001727
- Corpus ID: 205064043
Medical assistance in dying: research directions
- S. Dierickx , Joachim Cohen
- Published in BMJ Supportive & Palliative… 1 November 2019
- Medicine, Law
25 Citations
Assisted dying around the world: a status quaestionis., psychological aspects of medical assistance in dying: a personal reflection, assisted dying and palliative care in three jurisdictions: flanders, oregon, and quebec., physician-assisted suicide and physician-assisted euthanasia: evidence from abroad and implications for uk neurologists, for, against, and beyond: healthcare professionals’ positions on medical assistance in dying in spain, becoming a medical assistance in dying (maid) provider: an exploration of the conditions that produce conscientious participation., providing medical assistance in dying: practice perspectives., reasons for requesting medical assistance in dying., health care providers’ early experiences of assisted dying in aotearoa new zealand: an evolving clinical service, involvement of palliative care in patients requesting medical assistance in dying., 13 references, euthanasia and public health, attitudes and practices of euthanasia and physician-assisted suicide in the united states, canada, and europe., involvement of palliative care in euthanasia practice in a context of legalized euthanasia: a population-based mortality follow-back study, attitudes and experiences of belgian physicians regarding euthanasia practice and the euthanasia law., exploring the experiences of bereaved families involved in assisted suicide in southern switzerland: a qualitative study, death by request in switzerland: posttraumatic stress disorder and complicated grief after witnessing assisted suicide, process and outcomes of euthanasia requests under the belgian act on euthanasia: a nationwide survey., mental health outcomes of family members of oregonians who request physician aid in dying., effects of euthanasia on the bereaved family and friends: a cross sectional study, how accurately is euthanasia reported on death certificates in a country with legal euthanasia: a population-based study, related papers.
Showing 1 through 3 of 0 Related Papers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Fam Physician
- v.64(9); 2018 Sep
Language: English | French
Providing medical assistance in dying
Offrir l’aide médicale à mourir.
To explore the experiences of the first cohort of physicians to offer medical assistance in dying (MAID) in British Columbia.
Qualitative study using semistructured, one-on-one interviews.
British Columbia.
Participants
Eight physicians who offered MAID in British Columbia in 2016.
The physicians were interviewed by telephone or by e-mail between 4 and 6 months after MAID was made legal in Canada, with follow-up in January 2017. Interviews were audiorecorded, transcribed, and analyzed through qualitative thematic analysis.
Main findings
Participants believed that MAID was rewarding and satisfying work. They explained that some of the structural and emotional challenges related to providing MAID included the following: the refusal of faith-based institutions to provide information about MAID to patients, as well as their refusal to allow assessments or deaths to occur on site; having to deny MAID to patients who did not qualify for it; disagreements with colleagues who did not support the provision of MAID; dealing with the grief of family and friends who were present at the death; and feeling like they were always on call. While a few participants thought that the legislative restrictions of Bill C-14 were appropriate in the beginning when MAID was first available in Canada, most would like to see changes to the legislation to make it more aligned with the intent of the Carter decision, including broadening the eligibility criteria to include mature minors and people with advanced psychiatric diagnoses, having the ability to honour advance directives, and removing the requirement of death being in the reasonably foreseeable future for patients with grievous and irremediable conditions.
Physicians in this study explained that providing MAID is rewarding work; however, there are many challenges that complicate their ability to offer MAID to patients. The current MAID legislation in Canada should be updated to better serve the needs of patients.
Résumé
Décrire l’expérience des 8 médecins qui ont été les premiers à fournir l’assistance à mourir (AMM) en Colombie-Britannique.
Type d’étude
Une étude qualitative à l’aide d’entrevues individuelles semi-structurées.
La Colombie-Britannique.
Huit médecins qui ont dispensé l’AMM en Colombie-Britannique en 2016.
Méthodes
Les médecins ont été interviewés au téléphone ou par courrier électronique entre 4 et 6 mois après la légalisation de l’AMM au Canada, avec un suivi en janvier 2017. Les entrevues ont été enregistrées et transcrites pour ensuite faire l’objet d’une analyse thématique qualitative.
Principales observations
Les participants estimaient qu’il était satisfaisant et gratifiant de fournir l’AMM. Ils mentionnaient avoir été confrontés aux défis d’ordre structurel et émotionnel suivants, en rapport avec le fait d’offrir l’AMM : le refus d’établissements confessionnels de fournir des renseignements aux patients sur l’AMM et de permettre qu’il y ait des évaluations de l’admissibilité ou des décès sur place; le fait de devoir refuser l’AMM aux patients qui ne s’étaient pas qualifiés; le fait de ne pas s’entendre avec les collègues qui n’approuvaient pas la fourniture de l’AMM; le fait d’être confrontés à la peine des amis et des membres de la famille qui étaient présents au moment du décès; et l’impression d’être constamment sur appel. Bien que quelques participants croyaient que les restrictions législatives du projet de loi C-14 étaient initialement appropriées lorsque l’AMM est devenue disponible au Canada, la plupart aimeraient qu’on apporte certains changements à cette loi pour qu’elle soit davantage conforme aux intentions de la décision Carter, par exemple un élargissement des critères d’admissibilité pour inclure des personnes mineures matures et celles qui souffrent d’une maladie psychiatrique avancée, le fait de pouvoir répondre à des directives préalables et la suppression du critère exigeant que la mort prévue survienne dans un délai raisonnablement court dans le cas de patients gravement et irrémédiablement malades.
Les médecins qui participaient à cette étude ont dit que le fait de dispenser l’AMM était une tâche gratifiante; toutefois, ils ont dû faire face à plusieurs défis qui ont compliqué leur capacité d’offrir l’AMM aux patients. Une mise à jour de la loi canadienne sur l’AMM serait souhaitable afin de mieux répondre aux besoins des patients.
On February 6, 2016, in the precedent-setting Carter v Canada , 1 the Supreme Court of Canada held that laws prohibiting medical assistance in dying (MAID) violated the right to liberty of the person, and that MAID ought to be legal in Canada. 2 , 3 Between the Carter decision and the day that the new MAID legislation (Bill C-14) received royal assent on June 17, 2016, individual patients who wanted to receive MAID each required a court approval. 4 The current MAID legislation in Canada allows competent adults (those aged 18 and older) who have a grievous and irremediable medical condition to make a voluntary request for assistance in dying. A grievous and irremediable medical condition is one where the person has a serious and incurable condition, the person is in an advanced state of irreversible decline in capability, the person’s condition or decline causes intolerable physical or psychological suffering that cannot be acceptably relieved, and a natural death has become reasonably foreseeable. 2 Physicians and nurse practitioners can provide MAID, and allied health professionals, pharmacists, and patient-support persons are able to assist.
The first case of MAID in Canada outside of Quebec was a 66-year-old woman with amyotrophic lateral sclerosis from Calgary, Alta, who flew to Vancouver, British Columbia (BC), for her death on February 29, 2016. 4 Partly owing to the media attention surrounding this first case, the 2 Vancouver physicians who were involved were joined by 6 other physicians in BC who were interested in providing aid in dying. This group of 8 formed a peer-support group and shared their knowledge, experience, and challenges as they started to provide assessments and assisted deaths for patients. They exchanged more than 1000 e-mail communications in this process, and held meetings in-person and over the telephone.
The federal government published an interpretation of the law to help clinicians understand the restrictions. 5 In addition to complying with the federal law in the Criminal Code, clinicians must also follow the standards and guidelines of their licensing bodies and the provincial group of the regulatory authority to which they belong (eg, Royal College of Physicians and Surgeons of Canada, the Canadian Nurses Association, or the Canadian Pharmacists Association). These are similar but not the same across the country. The participants in this study complied with the College of Physicians and Surgeons of British Columbia guidelines, which included the submission of all documentation to the coroner’s office. 6
There are a few reports about experiences with euthanasia requests from the Netherlands that suggest that such requests can be stressful for primary care physicians. 7 , 8 It is important to research all aspects of MAID implementation in Canada to ensure the development of best practices and the use of appropriate inclusion criteria and safety guards. This article describes the perspectives and experiences of 8 physicians who collectively represent the first cohort of providers to offer MAID in BC.
This research project used semistructured interviews to explore the experiences of a cohort of physicians who were among the first to provide MAID in Canada. When little is known about a subject, exploratory descriptive qualitative research is used to begin to understand characteristics of phenomena, upon which additional research and theorizing can be built. 9 Semistructured interviews with small sample sizes are especially suitable for this type of research because they allow researchers to extend the conversation beyond standard questions and to follow research participants’ leads into new areas of conversation. 10
Eight physicians were interviewed by telephone or by e-mail between 4 and 6 months after MAID was made legal in Canada, and the opportunity for the physicians to provide further information was offered in January 2017. The interviews were conducted by 2 medical resident investigators (S.H. and A.N.). One of the authors (E.W.) was also an interviewee, serving as a form of member checking. Interviews were audiorecorded and transcribed by a research assistant (M.K.). Identifying features were removed and the investigators (J.S., A.J., S.H., and A.N.) analyzed the interviews using thematic qualitative analysis. Identified themes were compiled and evaluated in the context of what was already known about the provision of MAID in jurisdictions where it is legal (eg, Oregon, the Netherlands, Belgium). Investigators had discussions through e-mail communications, teleconferences, and in-person meetings, and consensus was reached on the main themes. This research project was approved by the University of British Columbia Behavioural Research Ethics Board.
Of the 8 physicians who were interviewed, 3 were from greater Vancouver, 3 were from Victoria, and 2 worked in a small community on Vancouver Island. Seven were family doctors and 1 was a general internist. Their ages ranged from 37 to 64 years. There were 2 men and 6 women; 6 worked full-time and 2 worked part-time. Collectively, by the end of December 2016, the 8 physicians in this study had assessed 332 people who were seeking MAID and had completed 135 assisted deaths. Assessments and deaths took place in hospitals, homes, hospices, clinical offices, and outdoors. Most of the patients who received MAID were not patients who were previously known to the providing physicians. However, in one case in which it was the participant’s own patient who had received MAID, the participant explained that “in many ways they are less stressful, because I know the patient and family better than my referral patients.”
Most of the participants were supportive of MAID before it was legalized, a few had not thought about it much before the media attention around MAID, and 1 participant was opposed to MAID before its legalization. The following is a description of a conversation a participant had had with a colleague before the legalization of MAID: “[When] we knew that this was coming about, we looked at each other and we said, ‘Well, where are the providers? Perhaps we better become them.’” The participant who had made the transition from opposing to supporting MAID simply stated that once it became legal, “patient choice and rights trump my personal feelings.”
All 8 participants described the steep learning curve that they experienced once they decided that they were interested in offering MAID. There were few regulations and no protocols that were immediately in place after MAID was legalized, and the physicians took it upon themselves to become educated in standards of best practice from international jurisdictions where MAID was already implemented. Two physicians traveled to the Netherlands in January 2016 to learn from colleagues there, and 5 attended an international euthanasia conference in the Netherlands in May 2016. As described by one of the participants:
The most useful thing we did was go to the Netherlands and speak to providers there. We spent some time there and we read everything we could and we talked to providers in Oregon and Washington and just were sort of like sponges and soaked up any information we could get from anyone who was providing medical assistance in death, up to date.
Throughout the process, the participating physicians turned to each other to share knowledge and to provide mutual support while developing protocols. Many are currently involved in teaching other health care providers about MAID both locally and nationally.
The interviews with the participating physicians revealed the following common themes.
Providing MAID is rewarding work.
There was a strong consensus among participants that providing MAID was rewarding work. Each of the participants spoke about how meaningful the practice of MAID was to them and to their patients. As one participant stated:
I think when you see the patients that we see, it’s very clear that you’re doing an incredible service. And that’s wonderful. There isn’t a single moment when I see these patients that I don’t think, “Oh my God, I’m so happy to be here to help you.” So that’s tremendously reinforcing ... I’m very proud to be doing it, and as I say, it’s incredible work, really, for the patient.
To be able to fulfil someone’s dying wish—to be able to offer someone a comfortable death that would end the intense suffering—was described as both an honour and a responsibility. One participant explained that “being able to give someone this gift, people are incredibly thankful—the families, the patients—it’s a bit overwhelming.”
Another participant stated the following: “[The] work is so wonderful … to offer something that these patients really, really want and deserve and have the right to. And they are so grateful. Oh, my heavens, they’re so grateful.”
While each of the deaths was different, the gratitude that was offered by patients and support persons to the attending physician were similar.
Many considerable challenges complicated the ability to provide MAID.
There were many important structural and emotional challenges that complicated and delayed the ability to offer MAID. While each physician anticipated that some of the challenges would be mediated as MAID became a more normal part of Canadian health care, often considerable efforts were required to ensure that patients received the care that they needed. The dedication of these physicians to work through structural and emotional challenges to offer MAID reflected their belief that offering it was an important service.
Structural challenges: Four of the 8 participants talked about problems they encountered with faith-based institutions refusing to provide information to patients and not allowing assessments on site, as well as other facilities refusing to allow MAID on the premises. When discussing how this affected patients beyond the facility itself, a participant explained the following: “Our hospital is Catholic and does not allow MAID. This policy has a knock-on effect in the community by limiting the number of nurses willing to attend a person’s home to site an IV [intravenous] cannula.”
When facilities refused to allow MAID to occur on the premises, patients still accessed it, but they often had to be transported to another facility. When describing what it was like to move patients in order to offer MAID, one participant explained how complicated the process was:
She was completely ambulatory, into the hospital for a short stay admission for 4 hours to do MAID, but the short stay admission probably took me 16 hours to arrange because then I had to do in-services with the staff, where it’s going to occur, talk to the director of admissions, try and arrange a bed, verify the bed, confirm the bed, and then deal with pharmacy and how we were going to [do] this because [she was] not a patient in the system, because she’s an outpatient.
Other considerable challenges included privileges not being honoured, having to spend many hours traveling for assessments and care provision, navigating legal requirements, having a lack of protocols, fulfilling the onerous paperwork requirements, and having to educate other health care providers along the way. As being part of the first cohort of MAID providers, participants said the following:
Once it became legal, it was a matter of winding it all up to start. The challenges were putting in the time and the effort to get it going. I spent 2.5 hours, at least, with the pharmacist the first time he was going to drop medications with me. We devised the protocol … I used a form that nobody else had ever used because they had just been developed the week before .... [While supporting the logistical arrangements of patients] can be overwhelming, [the] actual patient involvement is fantastic. That’s really rewarding and that keeps me going. It’s the bureaucratic stuff that takes the stuffing out of you.
Emotional challenges: The most difficult and most common emotional challenge was having to deny MAID to people who desperately wanted it but did not qualify under the current legislation. Having to turn people away when they would have qualified for MAID under the Carter decision but did not under Bill C-14 was especially distressing. For example, a patient who suffers from a serious and irreversible condition such as dementia would have qualified under the Carter decision, but no longer qualifies under the more restrictive current legislation because the patient’s natural death is not in the “reasonably foreseeable” future. Having to deny MAID to such patients was described as distressing because while the suffering of the patient was likely to increase, they would not be eligible for MAID until their condition progressed to such a state that death was reasonably foreseeable; and by the time the prognosis of a patient with dementia reaches that point, he or she is likely unable to give consent, thus rendering the patient’s eligibility for MAID null. A participant described such patients as “people who are suffering but are excluded by the law.” Another participant explained the following:
Saying no to patients does not ever get easier .... It still feels like the worst part of this work because those patients have come seeking help and as a physician I very much want to help them. But I am clear when I cannot and will always work within the [current] law.
Other emotional challenges included disagreements with colleagues who did not support the provision of MAID, dealing with the grief of family and friends who were present at the time of death, and feeling like they were on call all the time. To work through these challenges, peer support was identified as essential. As the first cohort of physicians providing MAID in BC, and with few guidelines from the College during the first few months of its legality, they turned to each other to discuss difficult cases, to think about appropriate protocols, and for emotional support. While one participant did feel strongly about practising MAID alone so as to keep the experience “less medical” for the patients and their support persons, they all relied on their ability to have open conversations about the process with each other, based on the fundamental value that “none of us are going to put ourselves in a position where we’re doing something that we don’t think is right.”
The current MAID legislation in Canada should be updated.
While a few of the study participants thought that the legislative restrictions of Bill C-14 were appropriate for when MAID was first available in Canada, most would like to see changes to the legislation to make it more aligned with the intent of the Carter decision. In particular, they believe the eligibility criteria should be broadened to include mature minors and people with advanced psychiatric diagnoses, and they should have the ability to honour advance directives. Furthermore, participants thought that the qualifying requirement of death being likely in the reasonably foreseeable future should be removed for patients with grievous and irremediable conditions. Because reasonably foreseeable was not defined in the initial legislation, it had been up to individual physicians, often with legal advice, to determine what they defined as reasonably foreseeable. Since this study was conducted, Justice Paul Perell clarified in the 2017 court case A.B. v Canada that in formulating an opinion about whether a patient’s death is reasonably foreseeable, “the physician need not opine about the specific length of time that the person requesting [MAID] has remaining in his or her lifetime.” 11 This has expanded how physicians and nurse practitioners can apply the concept of reasonably foreseeable in practice.
In this study, all 8 physicians found providing MAID to be very rewarding, despite the logistical challenges. We anticipate that many of the challenges mentioned above will be mitigated as Canadian physicians and the public have more exposure to and experience with MAID. Over the course of the study, developments were made as health authorities and individual institutions created and posted protocols, hired new staff to facilitate access to MAID, and offered training sessions across Canada. The physicians in this study described some of the stress that they experienced due to the extra hours that they worked during the early stages of the implementation of MAID, as they and their patients tried to navigate various legal and medical systems.
Globally, there are social taboos related to assisted death. 12 We expect that as MAID becomes more socially acceptable and more readily available, both the number of physicians who are willing to offer MAID and the number of patients who request it will increase. In places like the Netherlands and Belgium, where MAID has been legal for years, assisted deaths account for 4% to 5% of all deaths. 13 , 14 In Canada, this would translate to roughly 12 000 MAID deaths per year. This means that the need for providers will continue to increase, and that training about both the referral process and the actual provision of MAID will also need to increase.
Limitations
This study was limited to inquiring into the experiences of 8 physicians from BC who were early adopters of MAID and the findings are not generalizable to the experiences of other physicians. However, as a new medical procedure for which guidelines are still being developed, we believe that it is imperative that research about all aspects of MAID be conducted and shared.
The most consistent theme throughout this research was that providing MAID was incredibly satisfying and rewarding work. The biggest emotional challenge that participants identified in relation to providing MAID was having to deny care to a patient who did not qualify, especially if the patient would have qualified under the Carter decision, but no longer did under the current Bill C-14 legislation. Logistical challenges included having to travel to see patients who were bedridden, onerous documentation requirements, a lack of administrative support for arranging the actual MAID process, and privileges being denied by care facilities. Trying to support patients who were in facilities where access to MAID was denied, especially when they were in faith-based facilities, was described as one of the most common and most frustrating challenges. In order to overcome barriers and to prevent feelings of isolation, logistical and emotional peer support from other providers was identified as very important.
Editor’s key points
- ▸ In Canada, it has now been more than 2 years since legislation was passed permitting medical assistance in dying (MAID). As MAID is a newer medical procedure, it is important that all aspects of its implementation in Canada be examined. This article describes the perspectives of 8 physicians who collectively represent the first cohort of MAID providers in British Columbia.
- ▸ These MAID providers experienced many challenges that complicated their ability to provide MAID: spending many hours traveling for assessments and care provision, navigating legal requirements, fulfilling the onerous paperwork requirements, and having to educate other health care providers. Trying to support patients who were in facilities where access to MAID was denied was described as one of the most frustrating challenges. Despite the many challenges, the physicians described providing MAID as rewarding.
- ▸ Peer support was essential for these physicians. During the first few months of MAID’s legality, they turned to each other to discuss difficult cases and appropriate protocols, as well as for emotional support.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Grab your spot at the free arXiv Accessibility Forum
Help | Advanced Search
Computer Science > Computer Vision and Pattern Recognition
Title: llava-surg: towards multimodal surgical assistant via structured surgical video learning.
Abstract: Multimodal large language models (LLMs) have achieved notable success across various domains, while research in the medical field has largely focused on unimodal images. Meanwhile, current general-domain multimodal models for videos still lack the capabilities to understand and engage in conversations about surgical videos. One major contributing factor is the absence of datasets in the surgical field. In this paper, we create a new dataset, Surg-QA, consisting of 102,000 surgical video-instruction pairs, the largest of its kind so far. To build such a dataset, we propose a novel two-stage question-answer generation pipeline with LLM to learn surgical knowledge in a structured manner from the publicly available surgical lecture videos. The pipeline breaks down the generation process into two stages to significantly reduce the task complexity, allowing us to use a more affordable, locally deployed open-source LLM than the premium paid LLM services. It also mitigates the risk of LLM hallucinations during question-answer generation, thereby enhancing the overall quality of the generated data. We further train LLaVA-Surg, a novel vision-language conversational assistant capable of answering open-ended questions about surgical videos, on this Surg-QA dataset, and conduct comprehensive evaluations on zero-shot surgical video question-answering tasks. We show that LLaVA-Surg significantly outperforms all previous general-domain models, demonstrating exceptional multimodal conversational skills in answering open-ended questions about surgical videos. We will release our code, model, and the instruction-tuning dataset.
| Subjects: | Computer Vision and Pattern Recognition (cs.CV); Artificial Intelligence (cs.AI) |
| Cite as: | [cs.CV] |
| (or [cs.CV] for this version) | |
| Focus to learn more arXiv-issued DOI via DataCite (pending registration) |
Submission history
Access paper:.
- HTML (experimental)
- Other Formats
References & Citations
- Google Scholar
- Semantic Scholar
BibTeX formatted citation
Bibliographic and Citation Tools
Code, data and media associated with this article, recommenders and search tools.
- Institution
arXivLabs: experimental projects with community collaborators
arXivLabs is a framework that allows collaborators to develop and share new arXiv features directly on our website.
Both individuals and organizations that work with arXivLabs have embraced and accepted our values of openness, community, excellence, and user data privacy. arXiv is committed to these values and only works with partners that adhere to them.
Have an idea for a project that will add value for arXiv's community? Learn more about arXivLabs .

IMAGES
COMMENTS
Keywords: History, Medical assistance in dying, Philosophy of dying, Euthanasia, Suicide. In Athens, 399 BCE, the Greek philosopher Socrates - imprisoned and sentenced to death by hemlock on the charges of impiety and corrupting Athenian youth - famously raised a cup of the poison to his lips. [ 1] Descriptions of Socrates' equanimity at ...
Medical aid in dying, on the other hand, is when a terminally ill patient takes a prescribed medication to achieve a death in line with their own values, regardless of their degree of suffering. "Importantly, the patient must be dying to participate in medical aid in dying," said Dr. Treem. "Medical aid in dying is a choice of death, not ...
Suicide, Assisted*. Terminal Care*. Medical Assistance in Dying has had a profound impact on palliative care providers and their practice. Communication training with access to resources for ethical decision-making and a review of legislation may help address new challenges. Further research is needed to understand palliative care pro ….
Medical assistance in dying: implications for health systems from a scoping review of the literature Jamie K. Fujioka1,2,3, Raza M. Mirza4,5, Christopher A. Klinger4,5 and Lynn P. McDonald6,7 Abstract Objective: Medical assistance in dying (MAiD) is the medical provision of substances to end a patient's life at their voluntary request.
Abstract. Much of the literature on aid-in-dying (AID) has drawn heavily on rights-based ethical and legal frameworks that emphasize patients' rights of self-determination in end-of-life decision-making. Less attention has focused on how terminally ill people actually experience such putative rights once they are legally authorized.
Physician assistance with dying, variably termed voluntary euthanasia, assisted suicide, or Medical Assistance in Dying (MAiD), has become increasingly available in multiple countries (Dyer, 2008; Orentlicher, 2016; Watson, 2009).Canada legalized such assistance through the passage of Bill C-14 in 2016, which amended the federal Criminal Code allowing physicians and nurse practitioners to ...
Medical Assistance in Dying comprises interventions that can be provided by medical practitioners to cause death of a person at their request if they meet predefined criteria. In June 2016, Medical Assistance in Dying became legal in Canada, sparking intense debate in the palliative care community.
The legalization of Medical Assistance in Dying (MAID) in Canada in 2016 has had important legal and ethical implications for healthcare institutions. Prior to 2016, any form of assisted suicide was strictly prohibited under Section 241 of Canada's Criminal Code. ... At the time of the writing of this paper she was a Research Assistant at the ...
The legal criteria for medical assistance in dying (MAiD) for adults with a grievous and irremediable medical condition were established in Canada in 2016. There has been concern that potentially reversible states of depression or demoralization may contribute to the desire for death (DD) and requests for MAiD. However, little is known about the emergence of the DD in patients, its impact on ...
Background: Medical assistance in dying (MAID) became legal in Canada in 2016. Although the legislation is federal, each province is responsible for establishing quality care. Objective: To explore patient, family, and health care provider (HCP) perspectives on MAID access and care delivery and improve regional MAID care delivery.Design: Qualitative exploratory.
Research overwhelmingly cites existential reasons as the primary motivations for requests for medical assistance in dying. 48 Family members who have watched their loved ones end their life with medical assistance concur; they describe "feelings of anger, impotence, desperation and hopelessness" as the primary contributors to their loved ...
Background Medical assistance in dying (MAiD) sparks debate in several countries, some of which allow or plan to allow MAiD where a mental disorder is the sole underlying medical condition (MAiD-MD). Since MAiD-MD is becoming permissible in a growing number of jurisdictions, there is a need to better understand the moral concerns related to this option. Gaining a better understanding of the ...
The papers describe the unique ethical challenges involved in creating care pathways to support access to a novel and morally contested clinical practice. ... The state of knowledge on medical assistance in dying for mature minors: The Expert Panel Working Group on MAID for Mature ... Journal of Pharmacy Practice and Research. 2020; 50 (2):117 ...
Abstract (232 words) Medical assistance in dying (MAiD) is a globally polarizing topic which often sparks debate. surrounding the ethical and moral dilemmas that arise with a life-ending intervention. To gain a. better understanding of this intervention, it is important to explore the experience of those most.
From the impression of the current state of research regarding MAiD practices, a number of shortcomings and needs in research can be identified and it is suggested that at least the following five are most directly addressable. Euthanasia and assisted suicide, both sometimes referred to as medical assistance in dying (MAiD), have in recent years become increasingly important concerns for ...
Journal of the American Geriatrics Society (JAGS) is the go-to geriatrics journal for clinical aging research including education, clinical practice and public policy. Abstract Many patients with dementia want the option of using medical aid in dying (MAID) to end their lives before losing decision-making capacity and other abilities that ...
Assisted dying is legally permitted in a number of jurisdictions, such as Canada, the Netherlands, Belgium, Luxemburg, Switzerland, and several American states. 1 To be eligible for medical assistance in dying (MAiD) in Canada, the requester has to be aged 18+, eligible for government-funded health services, capable of making healthcare ...
Physician aid in dying is a controversial subject raising issues central to the role of physicians. According to the American Medical Association, it occurs when a physician provides "the necessary means and/or information" to facilitate a patient's choice to end his or her life [].This essay's authors hold varying views on the ethics of aid in dying; thus, the essay explores the ...
California defines an aid in dying drug as something a person may self-administer to bring about his or her death "due to a terminal disease.". New Jersey's law is called Medical Aid in Dying for the Terminally Ill where terminally ill is defined within the act as having a prognosis of six months or less.
Providing medical assistance in dying. Assistant Professor in the Faculty of Social Work at the University of Calgary in Alberta. Clinical Professor in the Department of Family Practice at the University of British Columbia in Vancouver and a family physician who practises in women's health and assisted death. Family physician in Vancouver, BC.
Multimodal large language models (LLMs) have achieved notable success across various domains, while research in the medical field has largely focused on unimodal images. Meanwhile, current general-domain multimodal models for videos still lack the capabilities to understand and engage in conversations about surgical videos. One major contributing factor is the absence of datasets in the ...
Canada's legalization of Medical Assistance in Dying (MAiD) in 2016 has had important implications for nursing regulators. ... At the time of the writing of this paper she was a research assistant at the University of British Columbia in Kelowna. Catharine J. Schiller is licensed as a practicing Registered Nurse and non-practicing lawyer in ...
Medical Assistance in Dying (MAiD) for Persons Whose Sole Underlying Medical Condition is a Mental Disorder: Challenges and Considerations ... Head of Research, University Health Network Centre for Mental Health; Senior Scientist, Toronto General Hospital Research Institute, Toronto, Ontario. ... A Response to the CPA Position Paper on Training ...